- *Corresponding Author:
- B. Huang
Department of Obstetrics and Gynaecology, Shiyan Maternal and Child Health Hospital, Shiyan, Hubei Province 442300, China
E-mail: huawgpq600@163.com
| This article was originally published in a special issue, “Advanced Targeted Therapies in Biomedical and Pharmaceutical Sciences” |
Indian J Pharm Sci 2023:85(1) Spl Issue “57-61” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
To evaluate the effect of dexmedetomidine on patient recovery from anesthesia in gynecologic laparoscopic surgery. A total of 74 patients who underwent gynecological laparoscopic surgery in our hospital between January 2020 and March 2022 were recruited and assigned via random method to receive either 0.6 μg/ kg of saline (observation group) or 0.6 μg/kg of dexmedetomidine (experimental group) before anesthesia induction during gynecologic laparoscopic surgery, with 37 cases in each group. Outcome measures included postoperative indices (recovery time, awakening time, orientation recovery time and extubation time), Ramsay scores, hemodynamic indices (heart rate, mean arterial pressure, pulse oximetry) at different time points and postoperative adverse events. Dexmedetomidine resulted in significantly shorter respiratory recovery time, awakening time, orientation recovery time and extubation time vs. control treatment (p<0.05). The Ramsay scores in the experimental group were significantly higher than those in the observation group (p<0.05) after treatment. Patients receiving dexmedetomidine showed lower heart rate and mean arterial pressure levels and higher pulse oximetry levels at extubation and 15 min after extubation than the controls (p<0.05). The incidence of postoperative adverse reactions in the experimental group was significantly lower than that in the observation group (p<0.05). Dexmedetomidine effectively shortens the recovery time of respiration, awakening time, recovery time of orientation and extubation time in patients undergoing gynecological laparoscopy and maintains the hemodynamic stability of the body without increasing the risk of postoperative adverse events in patients.
Keywords
Dexmedetomidine, laparoscopy, anesthesia, gynecology
Minimally invasive laparoscopic techniques are widely used in clinical gynecology as a diagnostic and surgical method with established effectiveness in clinical practice[1]. Laparoscopic surgery is less invasive, results in less intraoperative bleeding and provides a faster postoperative recovery vs. open surgery[2]. However, gynecological laparoscopy requires the performance of carbon dioxide pneumoperitoneum, which may disrupt the patient's abdominal blood flow pathways, resulting in a strong stress reaction. This is frequently treated by increasing the dose of anesthesia, which leads to the use of excessive doses of anesthetic drugs and thus compromises the recovery of the patient’s consciousness after surgery[3]. Therefore, there exists an urgent need to explore an effective anesthetic drug that inhibits the stress response of the patient without impairing the hemodynamics of the patient and the postoperative awakening effect[4]. Dexmedetomidine is a new alpha (α) 2-adrenergic agonist with good anesthetic effects. Research has reported a stable patient condition without increased risks of adverse events such as respiratory depression after the administration of dexmedetomidine[5]. To this end, this study was undertaken to evaluate the effect of dexmedetomidine on patient recovery from anesthesia in gynecologic laparoscopic surgery.
Materials and Methods
General information:
In this study, 74 patients who underwent gynecological laparoscopic surgery in our hospital between January 2020 and March 2022 were recruited and assigned via random method to either an observation group or an experimental group, with 37 cases in each group. The baseline patient profiles of the patients, including age, height, weight and American Society of Anesthesiologists (ASA) classification were collected. The study was approved by the ethics committee of our hospital and all patients and their families signed the relevant informed consent forms.
Inclusion and exclusion criteria:
Inclusion criteria: Patients were treated with gynecological laparoscopy in our hospital; with normal mental status and communication ability at the time of admission; aged ≥18 y old; with ASA classification of grade I-II; patients and family members were informed about the study and voluntarily participated.
Exclusion criteria: With a history of chronic pain; with dependence on or abuse of pain medications; with severe organ disease; with cardiovascular system disease; with contraindications related to surgery; with poor compliance that prevents good cooperation with this study and family members.
Treatment methods:
The patients fasted preoperatively. After entering the operating room, routine vital signs monitoring was performed and the patients received 0.5 mg of atropine, followed by the establishment of intravenous access.
Patients in the observation group received 0.6 µg/kg of saline by pump injection 30 min before anesthesia induction, while patients in the experimental group were given the same dose of dexmedetomidine by pump injection[6]. Rapid intravenous induction was performed and the patient received 0.04 mg/kg of imipramine+0.002 mg/kg of sufentanil citrate+2 mg/ kg of propofol+0.6 mg/kg of rocuronium bromide by intravenous infusion, followed by conventional tracheal intubation. Sevoflurane was used for anesthesia and the anesthesia was maintained until 5 min before the end of the operation. Patients were intermittently sedated with cisatracurium besylate intraoperative and, propofol and sufentanil were discontinued at the end of the operation, followed by the administration of the patient-controlled analgesia pump.
Outcome measures:
Postoperative indices: Postoperative indices (recovery time, awakening time, disorientation recovery time and extubation time) of patients in both groups were recorded.
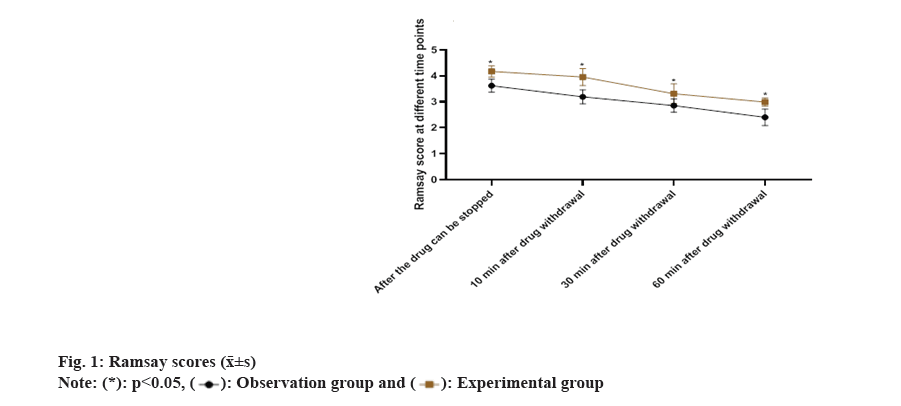
Ramsay scores: The Ramsay sedation scores were recorded in both groups immediately after drug discontinuation, 10 min after drug discontinuation, 30 min after drug discontinuation and 60 min after drug discontinuation. The Ramsay sedation score was 6 points in total, with <2 points for poor sedation, 2-4 points for ideal sedation and 5-6 points for excessive sedation[7].
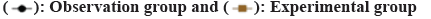
Hemodynamic indices: Heart Rate (HR), Mean Arterial Pressure (MAP) and Pulse Oximetry (SpO2) levels were recorded before drug administration, at extubation and 15 min after extubation in both groups.
Postoperative adverse events: The possible postoperative adverse events of patients include respiratory depression, nausea, vomiting and irritability.
Statistical analysis:
Statistical Package for the Social Sciences (SPSS) 22.0 was used for data analyses and GraphPad Prism 8 was used to visualize the data into corresponding images. The measurement data were expressed as mean±standard deviation (x̄ ±s) and examined using a t-test. The count data were expressed as the number of cases (rate) and tested using the Chi-square (χ2) test. p<0.05 indicates that the difference is statistically significant.
Results and Discussion
Patients in the observation group were aged 22- 47 (31.45±3.84) y, with a height of 155-173 (165.34±8.36) cm, a weight of 47-76 (61.44±6.25) kg and 22 cases of ASA class I and 15 cases of ASA class II. Patients in the experimental group were aged 21-45 (31.29±3.68) y, with a height of 154-171 (165.52±8.19) cm, a weight of 48-75 (61.59±6.32) kg and 21 cases of ASA class I and 16 cases of ASA class II. The patient characteristics between the two groups were comparable (p>0.05) as shown in Table 1.
| Observation (n=37) | Experimental (n=37) | t/χ2 | p | |
|---|---|---|---|---|
| Age (years) | 22-47 | 21-45 | ||
| Mean age (years) | 31.45±3.84 | 31.29±3.68 | 0.183 | 0.855 |
| Height (cm) | 155-173 | 154-171 | ||
| Mean height (cm) | 165.34±8.36 | 165.52±8.19 | -0.094 | 0.925 |
| Weight (kg) | 47-76 | 48-75 | ||
| Mean weight (kg) | 61.44±6.25 | 61.59±6.32 | -0.103 | 0.918 |
| ASA classification | 0.056 | 0.814 | ||
| I | 22 | 21 | ||
| II | 15 | 16 |
Table 1: Patient Characteristics (x̄±s, n (%))
Dexmedetomidine resulted in significantly shorter respiratory recovery time, awakening time, orientation recovery time and extubation time vs. control treatment (p<0.05) as shown in Table 2.
| Group | n | Respiratory recovery time | Awakening time | Orientation recovery time | Extubation time |
|---|---|---|---|---|---|
| Observation | 37 | 12.17±0.53 | 16.53±1.32 | 25.43±1.47 | 20.15±1.16 |
| Experimental | 37 | 8.42±0.38 | 13.84±0.95 | 21.34±1.53 | 18.04±0.98 |
| t | - | 34.977 | 10.061 | 11.725 | 8.452 |
| p | - | <0.001 | <0.001 | <0.001 | <0.001 |
Table 2: Postoperative Indices (x̄±s, min)
The Ramsay scores in the observation group were (3.62±0.25, 3.19±0.27, 2.85±0.26 and 2.40±0.32) immediately after drug discontinuation and 10, 30 and 60 min after drug discontinuation. The Ramsay scores of the experimental group were (4.17±0.22, 3.95±0.33, 3.31±0.38 and 2.99±0.16) immediately after drug discontinuation and 10, 30 and 60 min after drug discontinuation. The Ramsay scores in the experimental group were significantly higher than those in the observation group after treatment (p<0.05) as shown in fig. 1.
In the observation group, the HR was (80.34±4.92, 93.62±3.23, 83.51±5.32), MAP was (91.29±4.86, 99.23±6.27, 95.13±6.22) and SpO2 was (98.03±1.04, 95.12±0.62, 96.21±0.74) in the experimental group before drug administration, at extubation and 15 min after extubation. In the experimental group, the HR was (80.28±5.07, 82.26±4.14, 80.52±3.63), MAP was (90.83±5.21, 93.09±7.12, 89.23±4.20), SpO2 was (97.63±0.67, 98.23±0.85, 98.16±0.82) in the experimental group before drug administration, at extubation and 15 min after extubation. No statistically significant differences were observed in the HR, MAP and SpO2 levels between the two groups of patients before drug administration (p>0.05). Patients receiving dexmedetomidine showed lower HR and MAP levels and higher SpO2 levels at extubation and 15 min after extubation than the controls (p<0.05) as shown in fig. 2.
The incidence of postoperative adverse reactions in the observation group was 24.3 % (9/37), including 2 cases of respiratory depression, 5 cases of nausea and vomiting and 2 cases of agitation. The incidence of postoperative adverse reactions in the experimental group was 2.7 % (1/37), including 0 cases of respiratory depression, 1 case of nausea and vomiting and 0 cases of irritability. The incidence of postoperative adverse reactions in the experimental group was significantly lower than that in the observation group (p<0.05) as shown in Table 3. Laparoscopic surgery is a minimally invasive treatment modality with widely recognized effects in multiple clinical fields[8].
| Group | n | Respiratory depression | Nausea and vomiting | Irritability | Total incidence (%) |
|---|---|---|---|---|---|
| Observation | 37 | 2 | 5 | 2 | 24.3 % (9/37) |
| Experimental | 37 | 0 | 1 | 0 | 2.7 % (1/37) |
| c² | - | - | - | - | 7.4 |
| p | - | - | - | - | 0.007 |
Table 3: Postoperative Adverse Events (n (%))
Gynecologic laparoscopy is a minimally invasive procedure performed within a small operation port, thus avoiding the risk of injury and complications associated with previous open surgery[9]. In addition, this procedure allows for fine observation of the lesion under laparoscopic guidance, which contributes to avoiding traumatic areas during the surgery, thus reducing the risk of disease recurrence[10]. Moreover, this procedure obviate the need to open the patient’s abdomen, which effectively reduces intraoperative bleeding and the use of postoperative pain medication, thereby significantly improving the safety of the surgery[11]. However, special positions and the construction of a pneumoperitoneum are currently necessary for laparoscopic surgery, resulting in stimulation of the respiratory and cardiovascular systems and triggering a series of stress reactions[12]. Previously, opioids are commonly used for anesthesia, such as fentanyl, which effectively block the autonomic nerves and inhibit the stress response of the patient[13]. Nevertheless, it has been reported that opioids predispose patients to respiratory depression and prolong postoperative awakening time, resulting in limitations in their clinical use[14].
Dexmedetomidine, a new clinical α2-adrenergic agonist, has been proven to achieve desirable analgesic effects[15,16]. A study indicated that dexmedetomidine also offers faster onset of action[17], longer duration of maintenance, less dependence and milder respiratory depression than opioids. In addition, dexmedetomidine exerts a certain antagonistic effect on the adverse reactions caused by anesthetic drugs. Research indicated that dexmedetomidine exerts effects on A2A Adenosine Receptor (A2AAR) [18], spinal and peripheral a2AAR and a2ACR in locus coeruleus, leading to significant analgesic, sedative and neuroprotective effects and its administration in patients undergoing laparoscopic surgery during the awakening period of general anesthesia effectively suppresses stress response in patients.
The results of the present study showed that dexmedetomidine resulted in significantly shorter respiratory recovery time, awakening time, orientation recovery time and extubation time vs. control treatment, which is consistent with the results of previous research[19]. Nonetheless, it has also been reported that dexmedetomidine had no implications for prolonged postoperative extubation and awakening time of patients[20]. Such discrepancy may be attributed to the different determination criteria and the sample size. Moreover, the Ramsay scores in the experimental group were significantly higher than those in the observation group after treatment, indicating that dexmedetomidine provides more sedative benefits in patients undergoing laparoscopic gynecological surgery. Song et al.,[21] indicated that 0.6 µg/kg of dexmedetomidine administered 30 min before induction of anesthesia could effectively ensure the intraoperative hemodynamic stability of patients and well inhibit the extubation reflex. Herein, patients receiving dexmedetomidine showed lower HR and MAP levels and higher SpO2 levels at extubation and 15 min after extubation than the controls (p<0.05), which is consistent with the results by Song et al., suggesting that an appropriate amount of dexmedetomidine effectively improved the recovery from anesthesia in patients undergoing gynecological laparoscopy without causing major hemodynamic fluctuations. Furthermore, the incidence of postoperative adverse reactions in the experimental group was significantly lower than that in the observation group, suggesting a high safety profile of dexmedetomidine. Dexmedetomidine effectively shortens the recovery time of respiration, awakening time, recovery time of orientation and extubation time in patients undergoing gynecological laparoscopy, and maintains the hemodynamic stability of the body without increasing the risk of postoperative adverse events in patients.
Authors’ contributions:
Shikun Niu and Yingping Xu contributed equally to this work.
Conflict of interests:
The authors declared no conflict of interests.
References
- Massoth C, Schwellenbach J, Saadat-Gilani K, Weiss R, Pöpping D, Küllmar M, et al. Impact of opioid-free anaesthesia on postoperative nausea, vomiting and pain after gynaecological laparoscopy-A randomised controlled trial. J Clin Anesthesia 2021;75:110437.
[Crossref] [Google Scholar] [PubMed]
- Xue Y, Yuan H, Chen Y. Effects of dexmedetomidine as an adjunct in trans vs. abdominis plane block during gynecological laparoscopy. Exp Ther Med 2018;16(2):1131-6.
[Crossref] [Google Scholar] [PubMed]
- Li HJ, Liu S, Geng ZY, Li XY. Adding dexmedetomidine to morphine-based analgesia reduces early postoperative nausea in patients undergoing gynecological laparoscopic surgery: A randomized controlled trial. BMC Anesthesiol 2020;20(1):1-8.
- Wang X, Liu W, Xu Z, Wang F, Zhang C, Wang B, et al. Effect of dexmedetomidine alone for intravenous patient-controlled analgesia after gynecological laparoscopic surgery: A consort-prospective, randomized controlled trial. Medicine 2016;95(19):e3639.
[Crossref] [Google Scholar] [PubMed]
- Kang Y, Ni J, Wu L. Dexmedetomidine sedation combined with epidural anesthesia for laparoscopy in a patient with suspected tuberculosis: A case report. Medicine 2018;97(35):e12144.
[Crossref] [Google Scholar] [PubMed]
- Techanivate A, Dusitkasem S, Anuwattanavit C. Dexmedetomidine compare with fentanyl for postoperative analgesia in outpatient gynecologic laparoscopy: A randomized controlled trial. J Med Assoc Thai 2012;95(3):383.
[Google Scholar] [PubMed]
- Lozano-Díaz D, Valdivielso Serna A, Garrido Palomo R, Arias-Arias Á, Tarraga Lopez PJ, Martinez Gutierrez A. Validation of the Ramsay scale for invasive procedures under deep sedation in pediatrics. Pediatr Anesth 2021;31(10):1097-104.
[Crossref] [Google Scholar] [PubMed]
- Choi H, Song JY, Oh EJ, Chae MS, Yu S, Moon YE. The effect of opioid-free anesthesia on the quality of recovery after gynecological laparoscopy: A prospective randomized controlled trial. J Pain Res 2022:2197-209.
- Qin Z, Xiang C, Li H, Liu T, Zhan L, Xia Z, et al. The impact of dexmedetomidine added to ropivicaine for trans vs. abdominis plane block on stress response in laparoscopic surgery: A randomized controlled trial. BMC Anesthesiol 2019;19(1):1.
- Xiong X, Yang T, Shi Y, Shi J. Comment on: "Impact of opioid-free anaesthesia on postoperative nausea, vomiting and pain after gynaecological laparoscopy-A randomised controlled trial". J Clin Anesth 2021;75:110510.
[Crossref] [Google Scholar] [PubMed]
- Huang H, Xu X, Xiao Y, Jia J. The influence of different dexmedetomidine doses on cognitive function at early period of patients undergoing laparoscopic extensive total hysterectomy. J Healthc Eng 2021;2021:3531199.
[Crossref] [Google Scholar] [PubMed]
- McQueen-Shadfar LA, Megalla SA, White WD, Olufolabi AJ, Jones CA, Habib AS. Impact of intraoperative dexmedetomidine on postoperative analgesia following gynecologic surgery. Curr Med Res Opin 2011;27(11):2091-7.
[Crossref] [Google Scholar] [PubMed]
- Hakim KY, Wahba WZ. Opioid-free total intravenous anesthesia improves postoperative quality of recovery after ambulatory gynecologic laparoscopy. Anesth Essays Res 2019;13(2):199-203.
[Crossref] [Google Scholar] [PubMed]
- Singla D, Parashar A, Pandey V, Mangla M. Comparative evaluation of dexmedetomidine and labetalol for attenuating hemodynamic stress responses during laparoscopic cholecystectomy in borderline hypertensive patients. Rev Esp Anestesiol Reanim 2019;66(4):181-8.
[Crossref] [Google Scholar] [PubMed]
- Wang F, Zhong H, Xie X, Sha W, Li C, Li Z, et al. Effect of intratracheal dexmedetomidine administration on recovery from general anaesthesia after gynaecological laparoscopic surgery: A randomised double-blinded study. BMJ Open 2018;8(4):e020614.
[Crossref] [Google Scholar] [PubMed]
- Geng ZY, Liu YF, Wang SS, Wang DX. Intra-operative dexmedetomidine reduces early postoperative nausea but not vomiting in adult patients after gynaecological laparoscopic surgery: A randomised controlled trial. Eur J Anaesthesiol 2016;33(10):761-6.
[Crossref] [Google Scholar] [PubMed]
- Salman N, Uzun Ş, Coşkun F, Salman MA, Salman AE, Aypar U. Dexmedetomidine as a substitute for remifentanil in ambulatory gynecologic laparoscopic surgery. Saudi Med J 2009;30(1):77-81.
[Google Scholar] [PubMed]
- Srivastava D, Solanki S, Pradhan K, Singh P. Ventricular extrasystole during peri-operative intravenous dexmedetomidine infusion. Ann Card Anaesth 2013;16(1):69.
[Crossref] [Google Scholar] [PubMed]
- Volkov PA, Churadze BT, Sevalkin SA, Volkova Y, Guryanov VA. Dexmedetomidine as a part of analgesic component of general anesthesia for laparoscopic operations. Anesteziol Reanimatol 2015;60(1):4-8.
[Google Scholar] [PubMed]
- Wu Y, Huang H, Zeng J, Li B, Lei X, Chen Y. Effect of dexmedetomidine in preventing shivering after general anesthesia for laparoscopic surgery: A randomized, single-blinded and placebo-controlled trial. Nan Fang Yi Ke Da Xue Xue Bao 2013;33(4):611-4.
[Google Scholar] [PubMed]
- Song JY, Choi H, Chae M, Ko J, Moon YE. The effect of opioid-free anesthesia on the quality of recovery after gynecological laparoscopy: Study protocol for a prospective randomized controlled trial. Trials 2021;22(1):1-8.
[Crossref] [Google Scholar] [PubMed]