- *Corresponding Author:
- Qiaoyan Gao
Nursing Department,
Weihai Central Hospital,
Weihai,
Wendeng
264400,
China
E-mail: lanting0821@163.com
| This article was originally published in a special issue, “Trending Topics in Biomedical Research and Pharmaceutical Sciences” |
| Indian J Pharm Sci 2022:84(1) Spl Issue “81-86” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
To investigate the effect of ticagrelor combined with acupuncture on myocardial infarction and its effect on levels of serum myocardial enzymes, cytokines and T lymphocytes. 90 patients with myocardial infarction were equally divided into observation and control groups. The observation group was treated with ticagrelor combined with acupuncture, while the control group was treated with ticagrelor only. Hemodynamic indexes, left ventricular parameters, serum myocardial enzyme levels, cytokine levels and T lymphocyte levels were analyzed. The incidence of cardiovascular events 1 mo and 3 mo after treatment was investigated. There were no significant differences in heart rate, left ventricular end systolic diameter, left ventricular end diastolic diameter, intermittent septum thickness and posterior wall of left ventricle between two groups (p>0.05), while systolic blood pressure, diastolic blood pressure, mean arterial pressure and left ventricular systolic pressure in the observation group decreased and left ventricular end-diastolic pressure increased (p<0.05). After treatment, the levels of serum myocardial enzymes, tumor necrosis factor alpha, interferon gamma, interleukin-6, interleukin-17, interleukin-21 and interleukin-23 of observation group were significantly lower than control group, while transforming growth factor beta and T lymphocyte levels were significantly higher (p<0.05). The incidences of cardiovascular events in observation group were 2.22 % and 4.44 %, 1 mo and 3 mo after treatment, while it was 4.44 % and 8.89 %, respectively, in control group (p<0.05).
Keywords
Ticagrelor combined with acupuncture, myocardial infarction, serum myocardial enzymes, cytokines, T lymphocyte
In recent years, clinical statistics show that the majority of patients with myocardial infarction are the middleaged and the elderly. The disease occurs rapidly and poses a serious threat to health and the prognosis of patients after treatment is relatively poor [1]. At present, Percutaneous Coronary Intervention (PCI) is one of the commonly used methods to treat patients with myocardial infarction. Although the clinical effect is ideal, patients need to take medicine for life after treatment and there may be occlusion again. According to traditional medicine, myocardial infarction belongs to the category of "chest stuffiness and heartache" and patients mainly show chest tightness and pain, even back pain, shortness of breath and insomnia, etc. In the clinical treatment process, acupuncture therapy has its unique advantages and characteristics in the treatment of myocardial infarction [2]. In addition, clopidogrel is often used to treat patients with myocardial infarction in clinic, but there are relatively few reports on ticagrelor treatment [3]. In this study, 90 patients with myocardial infarction were selected to explore the therapeutic effect of ticagrelor combined with acupuncture on myocardial infarction and its effects on levels of serum myocardial enzymes, cytokines and T lymphocytes.
Materials and Methods
General data:
From April 2018 to October 2020, 90 patients with myocardial infarction in our hospital were selected as research objects, including 58 male patients and 32 female patients, with an average age of 60.43±5.56.
Inclusion criteria: Meeting the diagnostic criteria of myocardial infarction and the first incidence of myocardial infarction; cardiac Magnetic Resonance Imaging (MRI) indicating acute/subacute stage of myocardial infarction with obvious evidence of vascular stenosis and infarction. The clinical data of patients are complete and accurate, and there are no contraindications of chemotherapy and other physical diseases; all subjects have signed the informed consent form.
Exclusion criteria: Myocardial infarction patients are not diagnosed by pathological biopsy and cytological diagnosis; patients who have received chemotherapy; patients with severe organ failure such as heart, liver and kidney; patients who cannot cooperate to complete this experiment. There was no significant difference in general clinical data of all patients, such as age, weight and other diseases (p>0.05). The follow-up experiment could be carried out.
Methods:
90 patients with myocardial infarction were equally divided into observation group and control group, in which observation group was treated with ticagrelor combined with acupuncture, while control group was treated with ticagrelor only.
Ticagrelor treatment: Ticagrelor (AstraZeneca Pharmaceutical Co., Ltd., National Medicine Permission Number J20130020), oral dose of 180 mg, twice a day, medication time of 3 mo [4].
Ticagrelor combined with acupuncture treatment: On the basis of taking ticagrelor, acupuncture points were selected, including Baihui, Neiguan (bilateral), Zusanli (bilateral) and Sanyinjiao (bilateral). The acupuncture retention time was 20 min and the handmanipulating of needle was performed once during the period. The acupuncture was performed once a day and 6 d a course, with 1 d between every 2 courses and a total of 4 courses [5].
Observation indicators and methods:
Comparative analysis of hemodynamic indexes in two groups: After treatment, 24 h dynamic electrocardiogram was performed in both groups [6] and Systolic Blood Pressure (SBP), Diastolic Blood Pressure (DBP), Mean Arterial Pressure (MAP), Left Ventricular Systolic Pressure (LVSP), Left Ventricular End-Diastolic Pressure (LVEDP), and Heart Rate (HR) were recorded simultaneously.
Comparative analysis of left ventricular parameters in two groups: After treatment, the patients in both groups were examined by color Doppler echocardiography [7] and the patients kept quiet and rested for 5 min between two examinations to maintain calm. The patient took the left lateral position. Left Ventricular End Systolic Diameter (LVESD), Left Ventricular End Diastolic Diameter (LVEDD), Intermittent Septum Thickness (IVS) and Posterior Wall of Left Ventricle (PWLV) were measured at the level of mitral chordae in the long axis section of parasternal left ventricle.
Comparative analysis of serum myocardial enzymes level in two groups: Before and after treatment, the elbow venous blood of patents of two groups was taken at 7:00 in the morning after overnight fasting. After centrifugation at 3500 r/min for 20 min, the supernatant was collected and stored in a refrigerator at -20? for later use. The levels of myocardial enzymes, including Aspartate Aminotransferase (AST), Lactate Dehydrogenase (LDH), Creatine Kinase (CK) and Creatine Kinase Myocardial Band (CKMB) were measured by automatic biochemical analyzer.
Comparative analysis of cytokines level in two groups: According to the method as shown in comparative analysis of serum myocardial enzymes level in two groups, the venous blood was centrifuged to collect serum and then the Tumor Necrosis Factor alpha (TNF-α), Interferon gamma (IFN-γ) and Transforming Growth Factor beta (TGF-β), Interleukin (IL)-6 (IL-6), IL-17, IL-21 and IL-23 were detected by enzyme-linked immunosorbent assay and were compared for analysis.
Comparative analysis of T lymphocytes level in two groups: According to the venous blood obtained by the method as shown in comparative analysis of serum myocardial enzymes level in two groups, the blood serum was collected by centrifugation. Then the values of Cluster of Differentiation (CD) 3 (CD3+), CD4+ and CD8+ in the blood samples of the two groups were measured by flow cytometry and the ratio of CD4+/ CD8+ was calculated.
Comparative analysis of cardiovascular events in two groups: Cardiovascular events include major cardiovascular events and minor cardiovascular events. The main cardiovascular events are cardiovascularrelated deaths, non-fatal myocardial infarction and non-fatal stroke; minor cardiovascular events refer to recurrent angina pectoris and heart failure. Patients were followed up for 1 mo and 3 mo after treatment, and the incidence of cardiovascular events was statistically analyzed.
Statistical methods:
All the data in this study were processed by Statistical Package for the Social Sciences (SPSS) 20.0 statistical analysis software (IBM Company, USA). The measurement data was expressed by mean±standard deviation (x?±s). The comparison between groups was made by one-way analysis of variance or repeated measurement variance analysis and the pairwise comparison between groups was made by Least Significant Difference (LSD) t test; the counting data was expressed by percentage (%) and the comparison between groups was analyzed by χ2; p<0.05 indicated statistically significant difference.
Results and Discussion
Hemodynamic indexes in the two groups were compared. There was no significant difference in HR between the two groups (p>0.05). Compared with control group, SBP, DBP, MAP and LVSP in observation group decreased, while LVEDP increased significantly, with statistical significance (p<0.05) (Table 1).
| Group | SBP (mm Hg) | DBP (mm Hg) | MAP (mm Hg) | LVSP (mm Hg) | LVEDP (mm Hg) | HR (beats/min) |
|---|---|---|---|---|---|---|
| Control group | 110.54±7.98 | 93.24±5.76 | 99.98±6.67 | 111.88±8.57 | 10.56±2.21 | 367±28 |
| Observation group | 94.45±6.80 | 80.09±5.64 | 86.65±7.65 | 96.45±4.54 | 9.11±1.98 | 356±21 |
| t value | 10.323 | 9.405 | 10.231 | 12.564 | 10.003 | 0.326 |
| p value | 0.002 | 0.001 | 0.001 | 0.001 | 0.001 | 0.543 |
Table 1: Comparative Analysis of Hemodynamic Indexes in two Groups (x?±s)
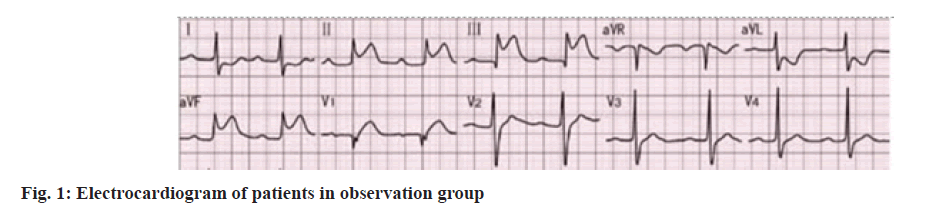
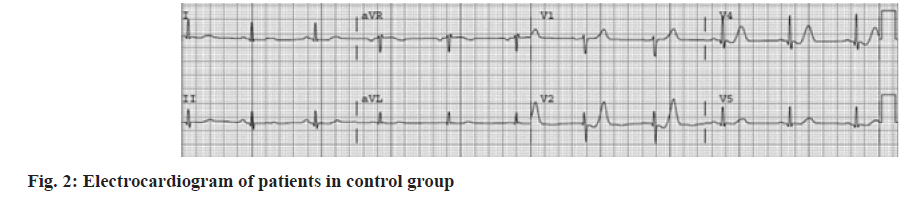
Left ventricular parameters in the two groups were compared. There was no significant difference in LVESD, LVEDD, IVS and PWLV between the two groups (p>0.05) (Table 2, fig. 1 and fig. 2).
| Group | LVESD | LVEDD | IVS | PWLV |
|---|---|---|---|---|
| Observation group | 30.88±4.68 | 43.98±5.66 | 10.75±2.10 | 9.52±1.26 |
| Control group | 29.69±3.39 | 43.54±3.15 | 10.63±1.12 | 9.37±2.38 |
| t value | 0.447 | 0.315 | 0.324 | 0.312 |
| p value | 0.372 | 0.791 | 0.477 | 0.870 |
Table 2: Comparative Analysis of Left Ventricular Parameters in two Groups (X?±S, Mm)
Serum myocardial enzymes level in two groups was compared. There was no significant difference in serum myocardial enzymes level between the two groups before treatment (p>0.05).
After treatment, serum myocardial enzymes level of patients in both groups decreased. Compared with patients in control group, serum myocardial enzymes levels (AST, LDH, CK and CKMB) of patients in observation group decreased significantly (p<0.05), with statistically significant difference (Table 3).
| Group | Index | Observation group | Control group | t value | p value |
|---|---|---|---|---|---|
| Before treatment | AST | 135.43±43.32 | 137.83±36.75 | 0.831 | 0.554 |
| LDH | 1023.43±109.21 | 1034.51±98.76 | 0.572 | 0.342 | |
| CK | 998.73±114.32 | 976.87±123.08 | 0.768 | 0.361 | |
| CKMB | 903.42±153.42 | 912.63±136.98 | 0.882 | 0.437 | |
| After treatment | AST | 112.16±11.31 | 127.45±8.76 | 9.023 | 0.002 |
| LDH | 812.07±61.15 | 974.23±48.46 | 8.651 | 0.001 | |
| CK | 704.06±30.55 | 820.49±34.43 | 9.992 | 0.001 | |
| CKMB | 754.43±35.89 | 822.12±76.54 | 6.547 | 0.002 |
Table 3: Comparative Analysis of Serum Myocardial Enzymes Level in two Groups (x?±s, U/l)
Comparative analysis of cytokines level in two groups of patients was shown here. Before treatment, there was no significant difference between the two groups (p>0.05). After treatment, the levels of cytokines in both groups showed significant changes. Compared with control group, the levels of cytokines (TNF-α, IFN-γ, IL-6, IL-17, IL-21 and IL-23) in observation group decreased, while the level of TGF-β increased significantly, with statistically significant difference (p<0.05) (Table 4).
| Group | Index | Observation group | Control group | t value | p value |
|---|---|---|---|---|---|
| Before treatment | TNF-α | 85.43±5.43 | 86.79±3.12 | 0.534 | 0.550 |
| IFN-γ | 93.21±4.44 | 94.45±5.09 | 0.672 | 0.439 | |
| TGF-β | 276.87±34.29 | 289.09±42.12 | 0.983 | 0.567 | |
| IL-6 | 156.32±27.86 | 162.31±33.41 | 0.447 | 0.531 | |
| IL-17 | 80.31±9.83 | 82.23±7.06 | 0.546 | 0.365 | |
| IL-21 | 178.93±54.42 | 181.34±48.98 | 0.482 | 0.672 | |
| IL-23 | 124.54±38.97 | 137.76±45.02 | 0.558 | 0.347 | |
| After treatment | TNF-α | 33.35±3.12 | 66.32±5.90 | 6.564 | 0.002 |
| IFN-γ | 32.84±6.22 | 78.23±8.01 | 16.112 | 0.001 | |
| TGF-β | 650.32±67.03 | 476.52±34.42 | 14.820 | 0.001 | |
| IL-6 | 77.45±6.12 | 103.44±12.54 | 17.217 | 0.001 | |
| IL-17 | 19.34±5.65 | 40.33±15.32 | 12.264 | 0.002 | |
| IL-21 | 81.88±5.32 | 120.34±16.53 | 9.632 | 0.001 | |
| IL-23 | 63.76±4.44 | 96.77±28.23 | 10.539 | 0.001 |
Table 4: Comparative Analysis of Cytokines Level in two Groups (X?±S, Ng/Ml)
T lymphocytes level in two groups was compared. Before treatment, there was no significant difference in T lymphocytes level between the two groups (p>0.05). After treatment, the level of T lymphocytes in both groups increased. Compared with control group, the levels of CD3+, CD4+, CD8+ and CD4+/ CD8+ in observation group significantly increased, with statistically significant difference (p<0.05) (Table 5).
| Group | Index | Observation group | Control group | t value | p value |
|---|---|---|---|---|---|
| Before treatment | CD3+ | 39.23±7.02 | 38.02±8.33 | 0.532 | 0.912 |
| CD4+ | 13.21±4.39 | 12.29±3.41 | 0.447 | 0.374 | |
| CD8+ | 14.21±3.92 | 13.88±2.56 | 0.512 | 0.463 | |
| CD4+/CD8+ | 0.48±0.14 | 0.46±0.29 | 0.983 | 0.527 | |
| After treatment | CD3+ | 72.34±3.45 | 56.65±1.87 | 7.442 | 0.002 |
| CD4+ | 42.35±4.12 | 26.12±3.65 | 7.512 | 0.001 | |
| CD8+ | 26.22±3.15 | 20.42±2.88 | 6.421 | 0.004 | |
| CD4+/CD8+ | 2.13±0.14 | 1.49±0.53 | 6.976 | 0.005 |
Table 5: Comparative Analysis Of T Lymphocytes Level in two Groups (X?±S, %)
Cardiovascular events in two groups were compared. The incidences of cardiovascular events in observation group were 2.22 % and 4.44 % 1 mo and 3 mo after treatment, while those in control group patients were 4.44 % and 8.89 %. Comparing the incidence of cardiovascular events between the two groups, the incidence of observation group was significantly less than that of control group, with statistically significant difference (p<0.05) (Table 6).
| Group | 1 mo after treatment | 3 mo after treatment | ||
|---|---|---|---|---|
| Number of cases | Incidence (%) | Number of cases | Incidence (%) | |
| Observation group (n=45) | 1 | 2.22 | 2 | 4.44 |
| Control group (n=45) | 2 | 4.44 | 4 | 8.89 |
| χ2 | 8.932 | 12.293 | ||
| p value | 0.004 | 0.001 | ||
Table 6: Comparative Analysis of Cardiovascular Events in two Groups
Myocardial infarction is a critical disease in cardiology and misdiagnosis often occurs due to the high risk of this disease. In addition, it also causes a series of complications, especially arrhythmia or heart failure [8]. Generally, coronary intervention is commonly used 6 h after the attack, so that ischemic myocardium can be reconstructed and dying myocardial cells can be saved to avoid further increasing the area of myocardial infarction [9]. Before coronary intervention, patients receive antiplatelet therapy to relieve blood viscosity and inhibit thrombosis. As an antithrombotic drug, ticagrelor has a remarkable antiplatelet effect. The clinical mechanism of this drug is similar to clopidogrel, but the difference is that there is an interaction effect between ticagrelor and platelet Purinergic Receptor (P2Y12) adenosine diphosphate receptor. In addition, it has certain reversibility and there is no conformation, and the signal transmission path has not changed. When the drug is stopped, the platelet function in the blood is obviously restored and the therapeutic effect is stable [10,11]. Acupuncture based on syndrome differentiation can warm yang, dispel cold, promote qi and remove blood stasis, and acupoints massaging can regulate the functions of yin and yang and viscera, so as to stimulate the heart-yang, regulate qi and relieve pain [12]. Clinical studies have found that massage at points such as Zusanli, Shenmen and Gongsun can relax vascular smooth muscle and relieve coronary spasm, thus improving the myocardial ischemia and hypoxia of patients [13].
The results of this study showed that SBP, DBP, MAP and LVSP of observation group patients decreased after treatment, while LVEDP increased significantly (p<0.05). In addition, levels of serum myogenic enzymes (TNF-α, IFN-γ, IL-6, IL-17, IL-21 and IL- 23) were significantly lower than those in control group, while TGF-β and T lymphocytes levels were significantly higher than those in control group (p<0.05). Clinical detection of serum myocardial enzymes is mainly used to judge whether patients have myocardial ischemia symptoms, including AST, LDH, CK and CKMB [14]. Among them, CK is the most important energy regulating enzyme in myocardium and CKMB is the isoenzyme of CK. At the same time, detection of the levels of CK and CKMB is helpful to accurately diagnose myocardial ischemia. Some scholars treated rats with electroacupuncture at Neiguan and Hegu points for 20 min, then stopped for 40 min and then resumed reperfusion after acupuncture at the same point for 20 min. Venous blood was collected and separated to obtain serum. It was found that the myocardial enzyme activity of rats in acupuncture treatment group decreased significantly, indicating that acupuncture at Neiguan and Hegu points could significantly inhibit myocardial enzyme activity [15]. Similarly, acupuncture was done at Neiguan and Shanzhong points of rats and the content of CK in rat serum was detected after eyeball blood collection. The results showed that acupuncture at Neiguan and Shanzhong points could obviously reduce the content of CK in rat blood [16]. New Zealand white rabbits were used for myocardial infarction modeling. Before the model was made, electroacupuncture or moxibustion at Neiguan point was adopted and then serum CK content was detected by enzyme-linked immunosorbent assay. The results showed that electroacupuncture and moxibustion pretreatment had preventive and protective effects on myocardial cells. They reduced serum CK content and both had delayed protective effects [17].
In addition, clinically, the changes of T lymphocytes level are generally reflected by detecting the changes of CD3+, CD4+, CD8+ and CD4+/CD8+ ratio, so as to judge the abnormal immune characteristics of myocardial infarction. T lymphocytes subsets mainly play an immunomodulatory role in CD4+ cells and CD8+ cells [18]. Usually, CD4+ and CD8+ interact to restrict and promote the immune function of the body in a balanced state. If the number and function of a certain T lymphocytes subgroup are abnormal, the body will suffer the disorder of immune system, which will lead to a series of pathological changes. Therefore, the change of CD4+/ CD8+ ratio is particularly important for clinical diagnosis of pathological infection [19,20]. The results of this study also showed that the incidences of cardiovascular events 1 mo and 3 mo after treatment were 2.22 % and 4.44 % in observation group and were 4.44 % and 8.89 % in control group (p<0.05). Therefore, the clinical safety of ticagrelor combined with acupuncture was better than that of ticagrelor alone.
To sum up, ticagrelor combined with acupuncture was effective and safe in treating myocardial infarction, which may be related to reducing serum myocardial enzymes level, inhibiting inflammatory cytokines expression and increasing T lymphocytes level. The combination of the two methods could improve patient’s myocardial infarction and promote the recovery of cardiac function. It is worthy of clinical application.
Conflict of interests:
The authors declared no conflict of interest.
References
- Ahn JH, Ahn Y, Jeong MH, Kim JH, Hong YJ, Sim DS, et al. Ticagrelor versus clopidogrel in acute myocardial infarction patients with multivessel disease; From Korea Acute Myocardial Infarction Registry-National Institute of Health. J Cardiol 2020;75(5):478-84.
[Crossref] [Google Scholar] [PubMed]
- Aytekin A, Ndrepepa G, Neumann FJ, Menichelli M, Mayer K, Wöhrle J, et al. Ticagrelor or prasugrel in patients with ST-segment-elevation myocardial infarction undergoing primary percutaneous coronary intervention. Circulation 2020;142(24):2329-37.
[Crossref] [Google Scholar] [PubMed]
- Ma CN. Correlation between inflammatory factor and endothelial function/platelet function in patients with acute myocardial infarction and rheumatoid arthritis. J Clin Cardiol 2018;34(5):468-72.
- Furtado RH, Nicolau JC, Magnani G, Im K, Bhatt DL, Storey RF, et al. Long-term ticagrelor for secondary prevention in patients with prior myocardial infarction and no history of coronary stenting: Insights from PEGASUS-TIMI 54. Eur Heart J 2020;41(17):1625-32.
[Crossref] [Google Scholar] [PubMed]
- Tateishi K, Saito Y, Kitahara H, Nakayama T, Fujimoto Y, Kobayashi Y. Increased platelet inhibition after switching from prasugrel to low-dose ticagrelor in Japanese patients with prior myocardial infarction. J Cardiol 2020;75(5):473-7.
[Crossref] [Google Scholar] [PubMed]
- Park Y, Koh JS, Lee JH, Park JH, Shin ES, Oh JH, et al. Effect of ticagrelor on left ventricular remodeling in patients with ST-segment elevation myocardial infarction (HEALING-AMI). Cardiovasc Interv 2020;13(19):2220-34.
[Crossref] [Google Scholar] [PubMed]
- Liu X, Baohua XU, Youhua WU. Change of inflammatory factors and its effect on prognosis in patients undergoing acute myocardial infarction thrombolysis treatment. Chin J Postgrad Med 2011;34(34):7-9.
- Gasecka A, Nieuwland R, Budnik M, Dignat?George F, Eyileten C, Harrison P, et al. Ticagrelor attenuates the increase of extracellular vesicle concentrations in plasma after acute myocardial infarction compared to clopidogrel. J Thromb Haemost 2020;18(3):609-23.
[Crossref] [Google Scholar] [PubMed]
- van der Hoeven NW, Janssens GN, Everaars H, Nap A, Lemkes JS, de Waard GA, et al. Platelet inhibition, endothelial function, and clinical outcome in patients presenting with ST?segment–elevation myocardial infarction randomized to ticagrelor versus prasugrel maintenance therapy: Long?term follow-up of the REDUCE?MVI trial. J Am Heart Assoc 2020;9(5):e014411.
[Crossref] [Google Scholar] [PubMed]
- Zhang Z, Nie XX. Effects of combined therapy of shexiang tongxin guttate pills and clopidogrel on platelet aggregation rate, hemorheology and helper T cell 1/2 balance in patients with acute myocardial infarction after undergoing percutaneous coronary intervention. World Clin Drug 2020;41(6):444-50.
- Liu ZM, Wang YS, Zhao SJ. Effect of thrombolytic therapy for acute myocardial infarction on serum TNF-α, IL-6 and sICAM-1 and its clinical significance. J Clin Res 2007;24(11):1898-900.
- Alexopoulos D, Sfantou D, Lianos I, Pappas C, Revela I, Triantafyllidi H, et al. Pharmacodynamic comparison of low-dose ticagrelor to low-dose prasugrel in patients with prior myocardial infarction: The ALTIC-2 study. Platelets 2020;31(6):812-4.
[Crossref] [Google Scholar] [PubMed]
- Li YJ, Ding WH, Shi LB. The influence of emergency percutaneous coronary intervention on plasma cytokines in acute myocardial infarction. Chin J Geriatr Heart Brain Vessel Dis 2006;4:231-3.
- Mar GY, Ridderstrale W, Wei J, Liu CP. Safety and cumulative incidence of major cardiovascular events with ticagrelor in Taiwanese patients with non-ST-segment elevation myocardial infarction: A 12-month, prospective, phase IV, multicenter, single-arm study. Acta Cardiol Sin 2020;36(3):195-206.
[Crossref] [Google Scholar] [PubMed]
- Zhang RY, Yang SS, Zheng WQ, Qiao ZY. Levels of blood lipid, inflammatory cytokines and prognosis of patients with acute coronary syndrome treated by percutaneous coronary intervention and rosuvastatin intensive treatment. Shanghai Med J 2016;39(7):391-95.
- Cesaro A, Taglialatela V, Gragnano F, Moscarella E, Fimiani F, Conte M, et al. Low-dose ticagrelor in patients with high ischemic risk and previous myocardial infarction: A multicenter prospective real-world observational study. J Cardiovasc Pharmacol 2020;76(2):173-80.
[Crossref] [Google Scholar] [PubMed]
- Buchtele N, Herkner H, Schörgenhofer C, Merrelaar A, Laggner R, Gelbenegger G, et al. High platelet reactivity after transition from cangrelor to ticagrelor in hypothermic cardiac arrest survivors with ST-segment elevation myocardial infarction. J Clin Med 2020;9(2):583-90.
[Crossref] [Google Scholar] [PubMed]
- Zhang L, Hu M, Chen Y, Wang Y. Effects of atorvastatin and ticagrelor combination therapy on renal function and the levels of suppression of tumorigenicity 2 and interleukin-33 in patients with ST-segment elevation myocardial infarction. J Int Med Res 2020;48(12): 300-307.
[Crossref] [Google Scholar] [PubMed]
- Zhang M, Hou JW, Wang XH, Liang M. Clinical effect of tirofiban combined with clopidogrel on acute myocardial infarction and the levels of IL-6, TNF-α and hs-CRP in serum. Hebei Med 2018;24(5):763-66.
- Dangas G, Baber U, Sharma S, Giustino G, Mehta S, Cohen DJ, et al. Ticagrelor with or without aspirin after complex PCI. J Am Coll Cardiol 2020;75(19):2414-24.
[Crossref] [Google Scholar] [PubMed]