- *Corresponding Author:
- S. Zhai
Physical Examination Centre, People's Hospital of Changyi City, Shandong Province,636 Limin Street, Changyi City, 261300, Shandong Province, China
E-mail: zhaisy_onco1@163.com
| This article was originally published in a special issue, "Clinical and Experimental Studies on Drug and Intervention Repurposing in China |
| Indian J Pharm Sci 2019:81(4)spl issue1;65-72 |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
In order to study the effect of health education intervention on women's concept and behavior of breast cancer screening, 600 women in urban and rural areas were investigated using a questionnaire. The subjects were randomly divided into experiment group and control group. The experiment group was given health education intervention related to breast cancer, and the control group was given health education intervention on common diseases except breast cancer. In the control group, the detection time was irregular, or no breast test was performed for more than one year. In the experimental group, after intervention, subjects underwent breast examination twice a year, and the patients with breast nodules were tested once every 3 months and 6 months. The results showed that the implementation of breast self-detection and breast clinical detection before health education intervention in the experiment group was increased and more regular, and the frequency was also increased. After health education unrelated to breast cancer, the implementation of breast self-detection and breast clinical detection in the control group increased, but it was not significant. It proves that this educational intervention model could help women improve their knowledge about early detection of breast cancer, and provide some help for improving women's prevention of breast cancer.
Keywords
Health education intervention, breast cancer, physical examination and screening
Nowadays, breast cancer has become one of the most common malignant tumours of women in the world and a leading cause of death[1-3]. But if breast cancer is detected early and treated regularly, the long-term cure rate is relatively high[4-6]. Breast cancer is one of the few malignant tumors that can reduce mortality through early screening. At present, there are no effective preventive measures for breast cancer. Only through early diagnosis and timely treatment of lesions can the mortality of patients be reduced and the quality of life of patients be improved[7,8]. Studies showed that breast cancer screening could reduce breast cancer mortality by 7 % in women aged 40-49 and 11 % in women aged 50-69. A general survey of asymptomatic women to detect, diagnose and treat breast cancer early is the key to reduce the mortality of breast cancer in the population[9]. At present, the American Cancer Association recommends the following three effective early screening methods for detection of breast cancer such as breast inspection (BSE), clinical breast examination (CBE), and mammography are for detecting breast cancer in asymptomatic women[10-13].
China has a large population, and although the incidence of breast cancer is very low, the total number of new breast cancer patients per year is second only to the United States, ranking second in the world[14]. Although many people suffer from breast cancer, there is still no recognized feasible scheme to promote the early detection of breast cancer in China, which makes Chinese women unable to regularly undergo breast cancer screening, and their awareness of early detection is also weak[15,16]. Though breast cancer screening has started in some big cities in China since the 1970s, the human, material and financial resources for screening are relatively limited. There are gaps and imbalances in technical equipment and people's cultural level between urban and rural areas and between different regions[17,18]. Therefore, an effective early detection plan should be formulated according to China's specific conditions and national conditions. Although BSE is considered to be a healthy behavior for early detection of breast cancer, the implementation of BSE in Chinese women is not optimistic[19]. Studies suggested that health education could improve women's knowledge, beliefs and attitudes towards BSE in the future, and promote inspection behaviour. However, with the passage of time, the number of people who insist on BSE gradually decreases[20]. Thus, regular health education for breast cancer prevention and adherence to BSE are the key to the success of secondary prevention of breast cancer.
In summary, breast cancer has become the primary problem of women's health in China. However, women in China lack knowledge of early detection of breast cancer, and the implementation rate of early detection is low. Therefore, it is very essential to improve women's awareness of breast cancer and promote implementation of early detection of health behaviour.
Materials and Methods
Research objective and data acquisition:
From January 2013 to January 2019, a total of 600 women aged 35 y from People's Hospital of Changyi City were selected as the research subjects. Then, according to the demographic variables (age, urban and rural distribution, marital status, educational level, and occupation), a control group was set up according to the principle of avoiding contamination. The experiment group received health education intervention, while the control group received different health knowledge education. In the control group, the detection time was irregular, or no breast test was performed for more than one year. In the experimental group, after intervention, subjects underwent breast examination twice a year, and the patients with breast nodules were tested once every 3 and 6 mo. After intervention with different health measures, the same group of subjects were surveyed again with the same questionnaire.
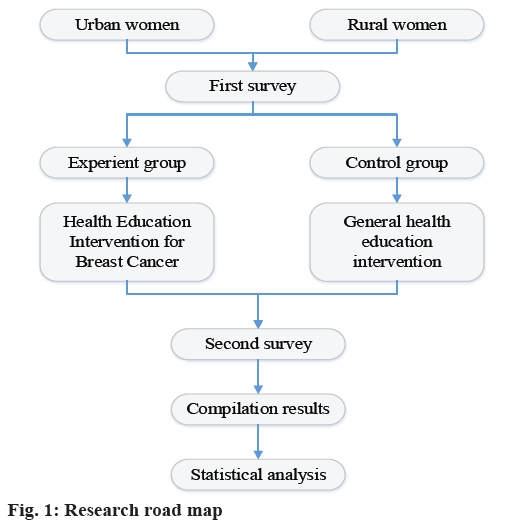
Research road map:
The research road map is shown in fig. 1. Based on the theory of health belief model (HBM), the experimental method of epidemiological field intervention and selfadministered questionnaire were used to organize the survey. Firstly, all the selected respondents conducted questionnaires on knowledge, BSE attitude and HBM of breast cancer prevention and health behaviour of breast early detection. Health education related to early detection of breast cancer was conducted in the experiment group, and in the control group, health education related to general diseases was carried out in women. Six months later, the same questionnaire was used to conduct a second survey in the original subjects. The changes of knowledge, attitude and behaviour of breast cancer prevention before and after intervention activities were compared between the experiment group and the control group, and the health education related to early detection of breast cancer was scientifically evaluated. Moreover, related factors affecting early detection of breast cancer in women were analysed.
Inclusion criteria and exclusion criteria:
Inclusion criteria: the permanent residence of the city, the population living in the area for six months; women aged 40 y and over, and women aged 35 y and over; those who have primary school and above education level, literacy and reading ability; mentally and physically healthy women without breast cancer symptoms. Those who volunteered to participate in the study, agreed and signed the informed consent after explanation.
Exclusion criteria included those who refused to participate in, patients with breast cancer or those who have undergone unilateral/bilateral breast cancer resection and currently in good health; those with a history of mental illness in the past and medical workers.
Survey method and questionnaire content:
Both the first and second surveys were cross-sectional surveys, which were conducted by the researchers themselves through self-filled questionnaires. At the beginning of the survey, women were asked to explain the purpose and significance of the study in detail, to explain the way and confidentiality of filling out the questionnaire, and women participated willingly. Questionnaires were distributed uniformly in class, filled in centrally and retrieved in class. In order to ensure true and reliable information, the questionnaire was anonymous. All questionnaires were retrieved and coded uniformly, and then statistics and analysis were carried out. The questionnaire was compiled according to China's actual situation and research objectives, and revised repeatedly on the basis of pre-experiment. It was revised into a questionnaire consisting of five parts, the birth date, urban and rural distribution, educational level, marital status, occupation and self-perceived health status of the respondents were investigated.
The knowledge of breast cancer and early detection of breast cancer was summarized as 16 closed-type nonselective questions. The content of the choice questions was mainly about the related important factors, symptoms and signs of breast cancer, how to detect breast cancer as early as possible, the significance of early detection of breast cancer, and the correct implementation methods. The available resources for conducting CBE examination were 6 closed singlechoice topics, including medical insurance for the respondents, opportunities for participating in health examination, time allowance, financial support, medical staff of breast examination in hospitals who often see doctors, and the equipment.
The attitude of BSE was surveyed with s7 closedchoice questions. The subjects' attitude toward BSE was assessed by Likert scale. According to the degree of acceptance of the questionnaires, the respondents were assigned 1-4 points from highly inactive to highly active. The health beliefs of early detection were divided into 4 sub-scales. There were 37 closed-choice questions, including the awareness of breast cancer susceptibility (5 questions), the awareness of breast cancer severity (8 questions), the awareness of the benefits of early detection of breast cancer (8 questions) and the awareness of early detection obstacles of breast cancer (21 questions). Each topic was assigned 1-5 points from very disagreeable to very agreeable.
Information sources, environmental impacts and family/social support for early detection of breast cancer: 23 closed-choice questions, 4 questions on information sources for early detection of breast cancer, 9 questions on the impact of environment on early detection of breast cancer in women, and 10 questions on family/social support. Early detection of breast cancer health behaviour, 11 closed-choice questions, the content of which was whether to implement and how to implement early detection behaviour.
Reliability and validity of questionnaires:
Cronbach's α reliability coefficient, which represents the internal consistency of the items in the questionnaire, is the most commonly used reliability coefficient at present. It shows the consistency of the scores of each item in the questionnaire. It is suitable for multiple scoring test data or questionnaire data. The reliability coefficient of α can explain how much of the variation of the score obtained by the scale test is determined by the true score, which reflects the extent of the scale affected by random errors and the reliability of the test. It is generally believed that >0.8 means good internal consistency, 0.6-0.8 is better, and <0.6 means poor internal consistency. The calculation formula is as follows, α = k/k–1(1–Σki=1S2i/S2T).
In the above formula, k is the total number of items in the scale, Si2 is the variance of the score of the i-th item, and ST2 is the variance of the total score. Construct validity: it is to understand the intrinsic attributes of a tool, reflecting the degree of integration between the tool and the theoretical or conceptual framework on which it is based. Structural validity is usually considered as the most powerful evaluation index of effectiveness. Factor analysis is often used to examine the structural validity of the scale. It is generally believed that the common factor of the scale can explain more than 50 % of the variation, and that each item has a sufficient load (≥0.4) on the corresponding factors, the scale has a good structural validity. Sample size estimation: according to the intervention effect of additional control in the field survey of health education, the calculation formula of sample size was obtained. n = (μα+ μβ)22p(1–p)/(p1–p2)2, where, p1 and p2 were estimated values before and after intervention, and p was merger rate.
Intervention contents of health education:
The experiment group, in order to ensure the effect of health education on early detection of breast cancer, the experiment group was divided into several groups according to the different communities of urban and rural areas and the respondents. The average number of health educators was about 30 simultaneously. Before health education, the questionnaire, atlas of early breast cancer detection, and record sheet of BSE were distributed centrally. Subjects were required to fill in questionnaires before lectures. The time of filling in the questionnaires was about 15 min. Then, health education on breast cancer early detection knowledge and methods of breast cancer early detection, especially the content of BSE methods, was carried out. The lectures were focused on videos of BSE, demonstrations and feedback with breast silica gel models, and lasted for about 2 h each time. After the health education activities, informed women about referring to books and BSE records and regularly adhering to the implementation of health behaviour. During the 6 mo study period, telephone follow-up, interviews and counselling were conducted according to the different educational levels of urban and rural respondents to know the implementation of early detection of breast cancer, and to answer women's questions. Each person was guided for an average of 1-2 times. After the 6 mo study, second evaluation was conducted, using the same tools as before.
Control group, the first survey was conducted with the same questionnaire, and then health education intervention was conducted for general diseases. The classroom focused on knowledge of hypertension, heart disease, diabetes, cancer and other common diseases, but did not involve knowledge of breast cancer. There was no atlas of early detection of breast cancer, only the records of BSE were issued. No intervention was given during the six-month study period, and the second evaluation was conducted half a year later, using the same questionnaire as before.
Statistical methods:
Each questionnaire recovered was numbered and the data entered into Excel spread sheet for sorting out and to import it into SPSS20.0 statistical software for analysis. Frequency and percentage were used to describe classification variables, and mean and standard deviation were used to describe continuous variables. P<0.05 showed that there was statistical significance. Descriptive analysis was used to reveal the distribution of research variables, such as women's general information, breast cancer prevention knowledge, HBM variables and breast cancer early detection behaviour. The changes between urban and rural areas, experiment group and control group, and before and after health education were compared by Chi-square test (Fisher's exact test if necessary) and Mann-Whitney U test. The multi-choice binary classification method was applied before the analysis of multiple-choice questions. To study the related factors affecting breast cancer early detection behaviour of urban and rural women, unconditional logistic regression analysis was used to determine the variables that have significant impact on breast cancer early detection health behaviour.
Results and Discussion
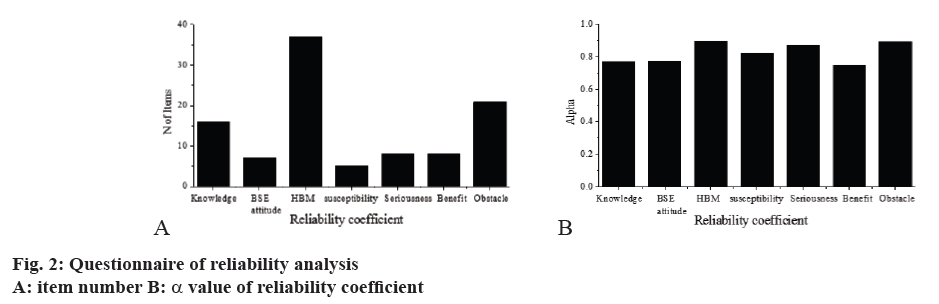
Four variables of knowledge, BSE attitude, health belief (HBM) and α coefficient of HBM as a whole were calculated, respectively. The statistics of α coefficient were shown in fig. 2. The reliability coefficient was between 0.747 and 0.897, indicating that the reliability was good, so the original content was not modified.
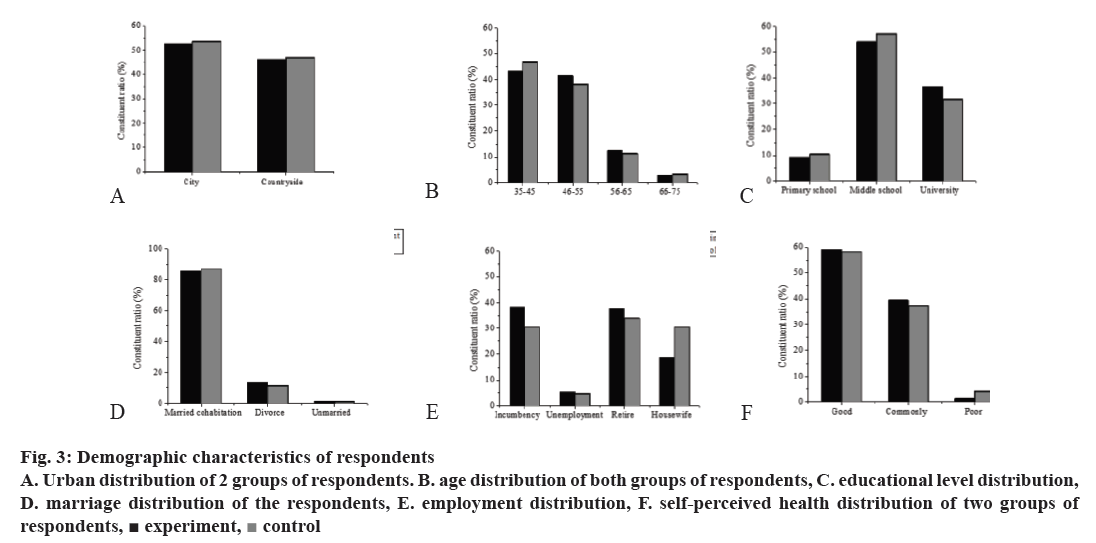
Among 600 respondents, 300 were in the experiment group and control group, respectively; 53.2 % were in urban areas and 46.8 % in rural areas; the age distribution of the respondents ranged from 35 to 80 y, with an average age of 49.8±9.13 y; only 9.8 % were in primary and lower-level schools; 12.3 % were divorced, widowed and unmarried in marital status; 28.8 % were in household women, 35.8 % were working women and 58.7 % were feeling good about their health. The baseline information of the experiment group and the control group was compared, as shown in fig. 3. There was no difference in the distribution of urban and rural areas, age stratification, educational level, marital status, occupation, and self-perceived health status between the two groups.
Figure 3: Demographic characteristics of respondents
A. Urban distribution of 2 groups of respondents. B. age distribution of both groups of respondents, C. educational level distribution,
D. marriage distribution of the respondents, E. employment distribution, F. self-perceived health distribution of two groups of
respondents,  experiment,
experiment,  control
control
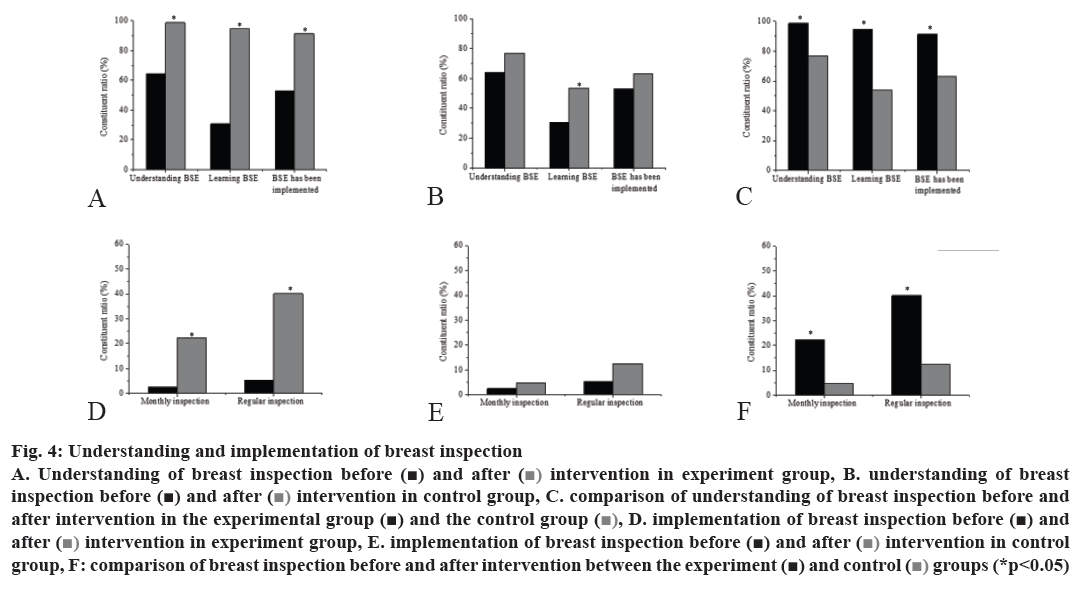
The women who had knowledge of BSE were 64.2 %, but only 30.6 % of women had studied BSE. There were many women who knew about BSE but had not implemented it, and 53.1 % of them did BSE. Only 2.5 % of the women had BSE every month, and only 5.3 % of the women had BSE regularly. From the data point of view, it is essential to improve women's BSE behaviour. Health education intervention was carried out in the experiment group, and statistics were applied again in the control group after general education. In the experiment group, 98.6 % of the people knew about BSE, 94.5 % learned about BSE, and 91.3 % implemented BSE. The number of women who had BSEs per month reached 22.4 %, and the number of women having regular BSEs reached 40.1 %. In the control group, 76.8 % knew about inspection of breast, 53.6 % learned about inspection of breast, and 63.2 % implemented inspection of breast. Only 4.7 % of the people did BSE monthly, and only 12.5 % did BSE regularly. As shown in fig. 4, 6 mo later, the understanding and implementation of BSE of experiment group was higher than those in the control group, and the difference was statistically significant. The proportion of BSE, regular BSE, and monthly BSE among BSE instructors who had received BSE at baseline and half a year later was higher than those who had not studied BSE. The difference was statistically significant, suggesting that it is very necessary to carry out health education for early detection of breast cancer.
Figure 4: Understanding and implementation of breast inspection
A. Understanding of breast inspection before ( ) and after (
) and after ( ) intervention in experiment group, B. understanding of breast
inspection before (
) intervention in experiment group, B. understanding of breast
inspection before ( ) and after (
) and after ( ) intervention in control group, C. comparison of understanding of breast inspection before and
after intervention in the experimental group (
) intervention in control group, C. comparison of understanding of breast inspection before and
after intervention in the experimental group ( ) and the control group (
) and the control group ( ), D. implementation of breast inspection before (
), D. implementation of breast inspection before ( ) and
after (
) and
after ( ) intervention in experiment group, E. implementation of breast inspection before (
) intervention in experiment group, E. implementation of breast inspection before ( ) and after (
) and after ( ) intervention in control
group, F: comparison of breast inspection before and after intervention between the experiment (
) intervention in control
group, F: comparison of breast inspection before and after intervention between the experiment ( ) and control (
) and control ( ) groups (*p<0.05)
) groups (*p<0.05)
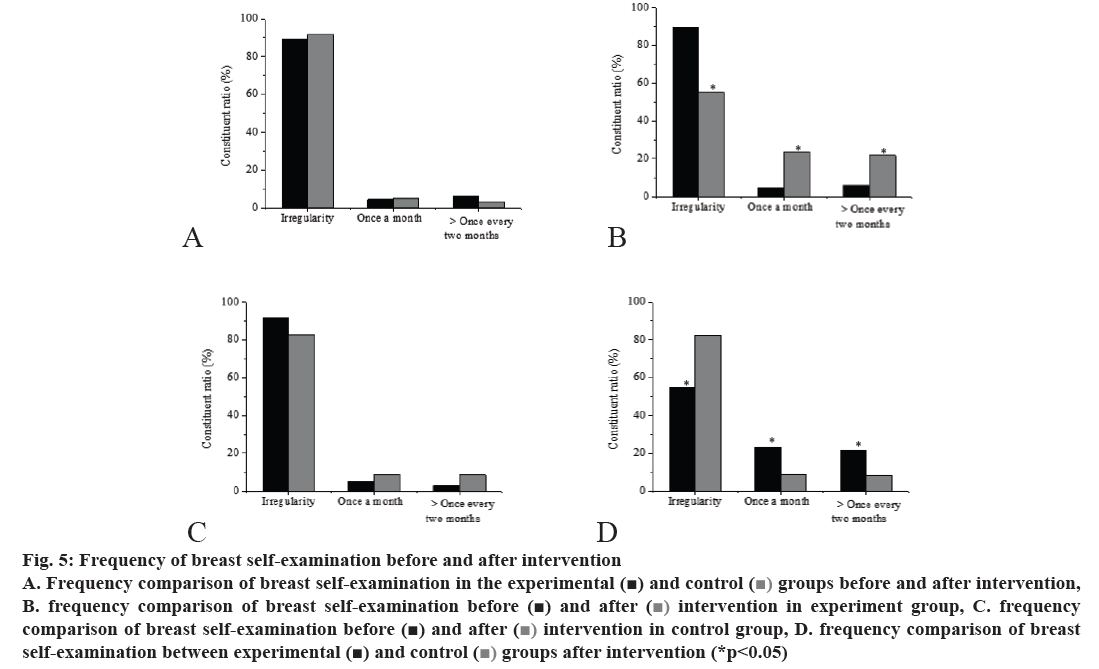
Comparing the frequency of BSE between the 2 groups, 89.3 % in the experiment group carried out BSE irregularly before education intervention, 4.6 % could make monthly BSE, and 6.1 % could make the BSE more than two months. After health intervention, the frequency of BSE in the experiment group dropped to 54.8, 23.3 % did it once a month, and 21.9 % did it once in more than 2 months; before education intervention, 91.7% in the control group carried out BSE irregularly, 5.1 % could make monthly BSE, and 3.2 % could make the BSE more than two months. After intervention, the rate of irregular BSE in the control group dropped to 82.5, 8.9 % did inspection once a month, and 8.6 % did it once in more than 2 mo. The results shown in fig. 5 indicated that there was no statistical difference between the 2 groups before and after education intervention. There was significant difference between the experiment group and the control group after health education intervention. The control group had no statistical significance before and after intervention. It suggested that health education intervention measures for early detection of breast cancer could help women regularly carry out BSE.
Figure 5: Frequency o f breast self-examination before and after intervention
A. Frequency comparison of breast self-examination in the experimental ( ) and control (
) and control ( ) groups before and after intervention,
B. frequency comparison of breast self-examination before (
) groups before and after intervention,
B. frequency comparison of breast self-examination before ( ) and after (
) and after ( ) intervention in experiment group, C. frequency
comparison of breast self-examination before (
) intervention in experiment group, C. frequency
comparison of breast self-examination before ( ) and after (
) and after ( ) intervention in control group, D. frequency comparison of breast
self-examination between experimental (
) intervention in control group, D. frequency comparison of breast
self-examination between experimental ( ) and control (
) and control ( ) groups after intervention (*p<0.05)
) groups after intervention (*p<0.05)
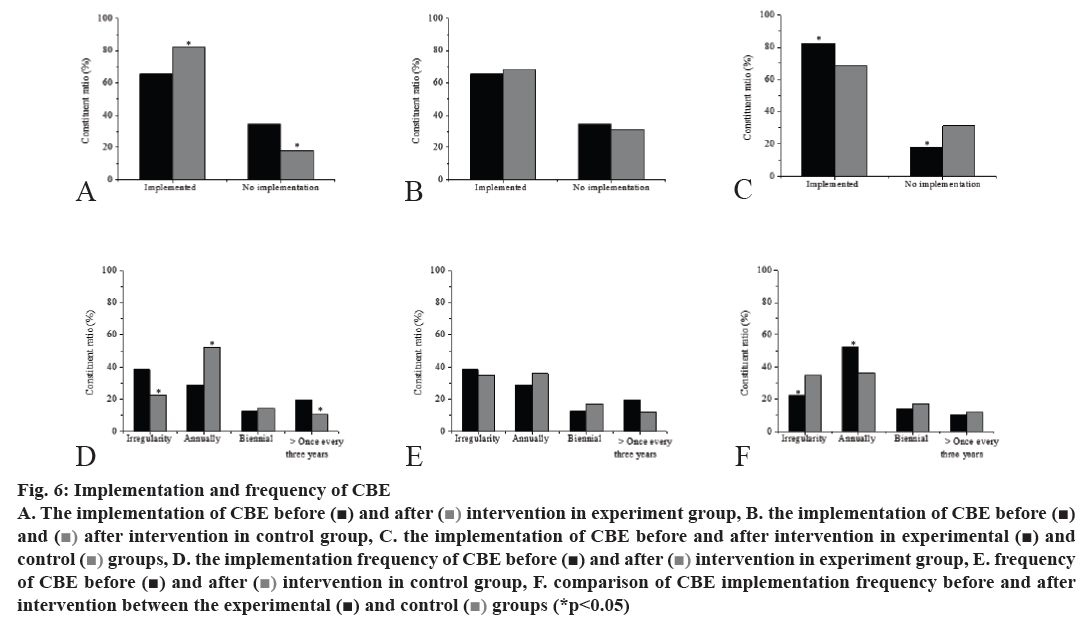
The frequency of CBE was compared between the two groups. The frequency of CBE before intervention was 65.5 %, irregular CBE was 38.4 %, the frequency of CBE reaching once a year was 29.1 %, the frequency of CBE every two years was 12.7 %, and the frequency of CBE more than 3 y was 19.8 %. After health intervention, 82.1 % of the experiment group had undergone CBE, 22.6 % had undergone CBE irregularly, 52.3 % had undergone breast examination every year, 14.4% had undergone CBE every 2 y, and 10.7 % had undergone CBE in more than 3 y. After intervention, 68.6 % of the patients in the control group had undergone CBE, 34.9% had undergone CBE irregularly, 36.1 % had undergone CBE once a year, 17.2 % had undergone CBE once every 2 y, and 11.8 % had undergone CBE once in more than 3 y. The results shown in fig. 6 indicated that there was no significant difference between the 2 groups before and after education intervention. There was significant difference in the experiment group before and after health education intervention, and there was also significant difference between the experiment group and the control group after intervention. The control group had no significant difference before and after intervention. It indicated that health education intervention measures for early detection of breast cancer were helpful to promote regular and more frequent CBE for women.
Figure 6: Implementation and frequency of CBE
A. The implementation of CBE before ( ) and after (
) and after ( ) intervention in experiment group, B. the implementation of CBE before (
) intervention in experiment group, B. the implementation of CBE before ( )
and (
)
and ( ) after intervention in control group, C. the implementation of CBE before and after intervention in experimental (
) after intervention in control group, C. the implementation of CBE before and after intervention in experimental ( ) and
control (
) and
control ( ) groups, D. the implementation frequency of CBE before (
) groups, D. the implementation frequency of CBE before ( ) and after (
) and after ( ) intervention in experiment group, E. frequency
of CBE before (
) intervention in experiment group, E. frequency
of CBE before ( ) nd after (
) nd after ( ) intervention in control group, F. comparison of CBE implementation frequency before and after
intervention between the experimental (
) intervention in control group, F. comparison of CBE implementation frequency before and after
intervention between the experimental ( ) and control (
) and control ( ) groups (*p<0.05)
) groups (*p<0.05)
This investigation studied the effect of health education intervention on improving the concept and behaviour of female breast cancer screening, and analysed the effect of health education intervention. The results showed that the implementation of breast self-detection and CBE before health education intervention in the experiment group increased and more regularly, and the frequency also increased. After health education unrelated to breast cancer, the implementation of breast self-detection and CBE in the control group increased, but it was not significant. There were significant statistical differences in detection frequency between the experiment group and the control group. It suggests that health education interventions for early detection of breast cancer can help women regularly and more frequently carry out breast self-examination and CBE. It proves that this educational intervention mode can help women improve their knowledge about early detection of breast cancer, and provide some help for improving women's prevention of breast cancer.
References
- Winters S, Martin C, Murphy D, Shokar NK. Breast Cancer Epidemiology, Prevention, and Screening. Prog Mol Biol Transl Sci 2017;151:1.
- Shah TA, Guraya SS. Breast cancer screening programs: Review of merits, demerits, and recent recommendations practiced across the world. J Microsc Ultrastruct 2017;5(2):59-69.
- Takkar N, Kochhar S, Garg P, Pandey AK, Dalal UR, Handa U. Screening methods (clinical breast examination and mammography) to detect breast cancer in women aged 40–49 years. J Midlife Health 2017;8(1):2.
- Shankar A, Roy S, Rath GK, Chakraborty A, Kamal VK, Biswas AS. Impact of Cancer Awareness Drive on Generating Understanding and Improving Screening Practices for Breast Cancer: a Study on College Teachers in India. Asian Pac J Cancer Prev 2017;18(7):1985-90.
- Evans RL, Pottala JV, Nagata S, Egland KA. Longitudinal autoantibody responses against tumor-associated antigens decrease in breast cancer patients according to treatment modality. BMC Cancer 2018;18(1):119.
- Esmail HE, Seedhom AE, Mahfouz EM. Awareness about Breast Cancer and Its Screening among Rural Egyptian Women, Minia District: a Population-Based Study. Asian Pac J Cancer Prev 2017;18(6):1623.
- Wachira J, Busakhala A, Chite F, Naanyu V, Kisuya J, Otieno G. Refining a questionnaire to assess breast cancer knowledge and barriers to screening in Kenya: Psychometric assessment of the BCAM. BMC Health Serv Res 2017;17(1):110.
- Reichart K. Lymphedema: Improving Screening and Treatment Among At-Risk Breast Cancer Survivors. Clin J Oncol Nurs 2017;21(1):21-5.
- Olasehinde O, Boutin-Foster C, Alatise OI, Adisa AO, Lawal OO, Akinkuolie AA, et al. Developing a Breast Cancer Screening Program in Nigeria: Evaluating Current Practices, Perceptions, and Possible Barriers. J Clin Res Oncol 2017;3(5):490-6.
- Jacobsen KK, Chelpin MVE, Vejborg I. Impact of invitation schemes on breast cancer screening coverage: A cohort study from Copenhagen, Denmark. J Med Screen 2017;24(1):20-6.
- Bahl M, Gaffney S, McCarthy AM, Lowry KP, Dang PA, Lehman CD. Breast Cancer Characteristics Associated with 2D Digital Mammography versus Digital Breast Tomosynthesis for Screening-detected and Interval Cancers. Radiology 2017;8(51):171148.
- Dogan BE, Scoggins ME, Son JB, Wei W, Candelaria R, Yang WT. American College of Radiology-Compliant Short Protocol Breast MRI for High-Risk Breast Cancer Screening: A Prospective Feasibility Study. AJR Am J Roentgenol 2017;210(1):1-8.
- Wu YT, Luo QQ, Li X, Arshad B, Xu Z, Ran L, et al. Clinical study on the prevalence and comparative analysis of metabolic syndrome and its components among Chinese breast cancer women and control population. J Cancer 2018;9(3):548-555.
- Wu KJ. Thoughts on optimizing the breast cancer screening strategies and implementation effects. Zhonghua Wai Ke Za Zhi 2018;56(2):101.
- Thomson MD, Peter ME. An opportunity to address modifiable breast cancer risks: Mammography screening and physical activity readiness to change. Prev Med Rep 2017;5(C):41-4.
- Savabi-Esfahani M, Taleghani F, Noroozi M. Role Playing for Improving Women’s Knowledge of Breast Cancer Screening and Performance of Breast Inspection. Asian Pac J Cancer Prev 2017;18(9): 2501-5.
- Lee HY, Mi HL, Jang YJ, Lee K. Breast Cancer Screening Disparity among Korean American Immigrant Women in Midwest. Asian Pac J Cancer Prev 2017;18(10):2663-8.
- Morjaria P, Bastawrous A, Murthy GVS, Evans J, Gilbert C. Effectiveness of a novel mobile health education intervention (Peek) on spectacle wear among children in India: study protocol for a randomized controlled trial. Trials 2017;18(1):168.
- Tawfik MY. The Impact of Health Education Intervention for Prevention and Early Detection of Type 2 Diabetes in Women with Gestational Diabetes. J. Community Health 2017;42(3):500-10.
- Hürlimann E, Silué KD, Zouzou F, Ouattara M, Schmidlin T, Yapi RB, et al. Effect of an integrated intervention package of preventive chemotherapy, community-led total sanitation and health education on the prevalence of helminth and intestinal protozoa infections in Côte d’Ivoire. Parasites Vectors 2018;11(1):115.