- *Corresponding Author:
- Baojin Zeng
Department of Obstetrics and Gynecology, Taizhou Hospital of Zhejiang Province, Affiliated to Wenzhou Medical University, Taizhou, Zhejiang Province 317000, China
E-mail: zengbj@enzemed.com
| Date of Submission | 05 January 2021 |
| Date of Revision | 14 July 2021 |
| Date of Acceptance | 30 May 2022 |
| Indian J Pharm Sci 2022;84(3):676-682 |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
To assess the effects of cluster of differentiation 147 on the proliferation, migration and invasion of cervical cancer HeLa cells by inhibiting its expression using short hairpin ribonucleic acid. A total of 110 cases of cervical tissues, including 20 cases of normal cervical epithelial tissues and 90 cases of cervical cancer tissues (30 cases of cervical cancer in situ tissues and 60 cases of cervical squamous cell cancer tissues) stored in our hospital from February 2016 to February 2019 were selected. The expression of cluster of differentiation 147 was detected by immunohistochemistry. Then the correlations of cluster of differentiation 147 expression with clinicopathological parameters such as age, tumor size, invasion depth, clinical stage and lymphatic metastasis of cervical cancer patients were analyzed. Control and experimental groups were transfected with green fluorescent protein-short hairpin ribonucleic acid-cluster of differentiation 147-negative control and green fluorescent protein-short hairpin ribonucleic acid-cluster of differentiation 147, respectively and blank cells were set as normal group. Cell proliferative ability was measured through 5-ethynyl-2'- deoxyuridine labeling assay and the migratory and invasive abilities of the cells were determined using Transwell assay. Western blotting was performed to detect the protein expressions of monocarboxylate transporter 1 and cluster of differentiation 147. The positive expression rate of cluster of differentiation 147 in cervical cancer in situ tissues significantly increased compared with that in normal cervical tissues, which was significantly higher in cervical squamous cell cancer tissues (p<0.05). The expression of cluster of differentiation 147 was not associated with the age and clinical stage of cervical cancer patients (p>0.05), but had close correlations with the tumor size, invasion depth or lymphatic metastasis of cervical cancer patients (p<0.05). Compared with normal group, the proliferative, migratory and invasive abilities of cells were significantly weakened and the protein expressions of monocarboxylate transporter 1 and cluster of differentiation 147 were significantly down-regulated in experimental group (p<0.05). The expression of cluster of differentiation 147 is increased in cervical cancer tissues and inhibiting such expression can prominently decrease the proliferative, invasive and migratory abilities of tumor cells in vitro and in vivo.
Keywords
Cluster of differentiation 147, short hairpin ribonucleic acid, cervical cancer, proliferation, migration, invasion
Cervical cancer is one of the common reproductive system malignancies, of which the cancer in situ frequently occurs at the age of 20-45 y old, while invasive squamous cell cancer has a high incidence rate among people aged 45-55 y old. Cervical cancer is a leading cause of cancer-related death of females and its morbidity and mortality rates are particularly higher in developing regions. Since the disease has an insidious site and no typical clinical symptoms in the early stage and rapidly progresses due to ultra-strong malignant proliferation and target organ metastasis of tumor cells, most patients have been in the intermediate and advanced stage when definitely diagnosed, missing the best timing for surgical resection[1]. The recurrence and malignant invasion of tumor are important causes of death of patients with intermediate and advanced cervical cancer[2]. Hence, actively exploring the specific molecular markers for cancer cell proliferation and metastasis from the perspective of molecular mechanism of the disease is not only beneficial to the early diagnosis of cervical cancer, but also conducive to conducting targeted therapy and reducing mortality rate of patients. Extracellular Matrix Metalloproteinase (MMP) inducer, also known as Cluster of Differentiation 147 (CD147), is a transmembrane glycoprotein in the immunoglobulin superfamily. CD147 can enhance MMP expression in tumor cells and promote the infiltration, invasion, adhesion and malignant metastasis of cancer cells[3]. The expression of CD147 is raised in multiple malignant tumors including laryngeal squamous cell carcinoma, nonsmall cell lung cancer, breast invasive ductal carcinoma and ovarian cancer, and tumor patients with a high CD147 expression have a poor prognosis[4]. However, the role of CD147 in cervical cancer is rarely reported. Short hairpin Ribonucleic Acid (shRNA) refers to an RNA interference technique for silencing target gene expression by means of gene technology[5]. In this study, the expression of CD147 in cervical cancer was detected by researching the clinical tissue samples of cervical cancer and cancer cells, and its influences on the proliferation, invasion and metastasis of cervical cancer cells were investigated, aiming to provide reliable target sites for targeted therapy of cervical cancer in clinic.
Materials and Methods
Data of clinical tissue samples:
A total of 110 cases of cervical tissues, including 20 cases of normal cervical epithelial tissues and 90 cases of cervical cancer tissues (30 cases of cervical cancer in situ tissues and 60 cases of cervical squamous cell cancer tissues) stored in the pathological tissue room of our hospital from February 2016 to February 2019 were selected. Before sample collection, all patients were diagnosed with cervical cancer for the first time and none of them received radiotherapy, chemotherapy, immunotherapy or endocrine therapy for intervention. It was found through statistical analysis that there were no significant differences in age, childbearing or not, body height and body weight of patients (p>0.05). The patients or their families were informed of the study protocol and objective, and signed the informed consent. This study was reviewed and approved by the Ethics Committee of the Zhejiang Taizhou Hospital Affiliated to Wenzhou Medical University.
Cells and main reagents:
Cervical cancer HeLa cell line was provided by American Type Culture Collection. RNA interference technique and the plasmids for constructing adenovirusmediated Green Fluorescent Protein (GFP)-shRNACD147 and GFP-shRNA-CD147-Negative Control (NC) were offered by Shanghai GenePharma Co., Ltd.
Glyceraldehyde-3-Phosphate Dehydrogenase (GAPDH) and rat anti-rabbit antibodies against CD147 and Monocarboxylate Transporter 1 (MCT1) were purchased from Abcam (USA). Kits for 5-Ethynyl-2'-deoxyuridine (EdU) labeling assay, immunohistochemistry, Transwell assay and Western blotting were bought from Shanghai Beyotime Biotechnology Co., Ltd. In addition, micropipette (Eppendorf, Germany), intelligent incubator (SANYO, Japan), IXplore Standard inverted microscope (Olympus, Japan), real-time fluorescence quantitative Polymerase Chain Reaction (PCR) instrument (ABI, USA), fluorescence microscope (Nikon, Japan) and gel imaging system (UVP, USA) were employed.
Detection of CD147 expression in clinical samples by immunohistochemistry:
The sample tissues were routinely fixed, embedded in paraffin and sliced to 4 μm-thick sections for retrieval with citric acid buffer solution and blocking with hydrogen peroxide. Then the tissues were incubated with primary antibodies in a cassette at 4° overnight and added with secondary antibodies, followed by color development, cleaning, counterstaining, dehydration, transparentization, mounting and microscopic examination. The yellowish-brown granules in the field of vision indicated positive results[6]. Positive or negative expression of CD147 was judged based on the staining intensity and percentage of positive cells in 5 fields of vision randomly selected from each sample by two senior pathological researchers. Moreover, the correlations of CD147 expression with clinicopathological parameters such as age, tumor size, invasion depth, clinical stage and lymphatic metastasis of patients were analyzed.
Cell transfection:
After thawing, HeLa cells were inoculated into a Dulbecco's Modified Eagle Medium (DMEM) containing inactivated 10 % Fetal Bovine Serum (FBS) and cultured in a constant-temperature and constanthumidity biochemistry incubator with 5 % Carbon dioxide (CO2) at 37°. The experiment was initiated when the cell density reached 85 %. The cells in control group and experimental group were transfected with GFP-shRNA-CD147-NC and GFP-shRNA-CD147, respectively and blank cells were set as normal group.
All the three groups of cells were routinely cultured for 24 h and the transfection efficiency was determined using the PCR instrument.
Observation of morphological changes of cells:
The cells were seeded into 6-well culture plates at 5×104 cells/well after concentration adjustment and subjected to the aforementioned grouped treatments. Next, the cells were routinely cultured in the constanttemperature and constant-humidity biochemistry incubator for 24 h after gentle mixing, fixed with 10 % formaldehyde and observed under an inverted phasecontrast microscope.
Detection of proliferative ability of cells by EdU labeling assay:
After concentration adjustment, the cells were seeded into 6-well culture plates at 5×104 cells/well and received the same grouped treatments as mentioned above. Next, the cells were routinely cultured in the constant-temperature and constant-humidity biochemistry incubator for 24 h after gentle mixing, fixed with 10 % formaldehyde and subjected to the EdU labeling assay strictly according to the kit instructions.
Detection of migratory and invasive abilities of cells by Transwell assay:
A layer of Matrigel (about 50 μl) was paved onto the plate in the Transwell chambers, the single-cell suspension of the serum-free medium in each group was added into the upper chamber (Matrigel was paved in invasion assay instead of migration assay) and the lower chamber was paved with the DMEM containing inactivated 10 % FBS, followed by routine culture in a 5 % CO2 incubator at 37° for 24 h. After washing, the chambers were fixed using formaldehyde, stained and observed under the microscope. Finally, the transmembrane cells were counted and recorded.
Detection of expression levels of CD147 and MCT1 in cells by Western blotting:
The cells were digested with trypsin, centrifuged and diluted into single-cell suspension, followed by the aforementioned grouped treatments. Then the cells were seeded into 6-well plates at 1×105 cells/well and cultured in the incubator with 5 % CO2 at 37° for 24 h. Later, protein lysate was added to extract total proteins from cells in each group. Next, the concentration was detected and the proteins were denatured in boiling water, separated by electrophoresis and transferred onto a membrane. After washing, the proteins were incubated with blocking buffer for 30 min, primary antibody (1:500) overnight and secondary antibody (1:1000), followed by color development with diaminobenzidine. Finally, the grayscale value of each band was statistically analyzed using ImageJ image analysis software with GAPDH as the internal reference.
Statistical analysis:
Statistical Package for the Social Sciences (SPSS) 19.0 software was used for statistical analysis of experimental data. The measurement data were represented as mean±standard deviation and analyzed by t-test. All the data conformed to normal distribution. The numerical data were analyzed by Chi-square (χ2) test. p<0.05 suggested statistically significant differences.
Results and Discussion
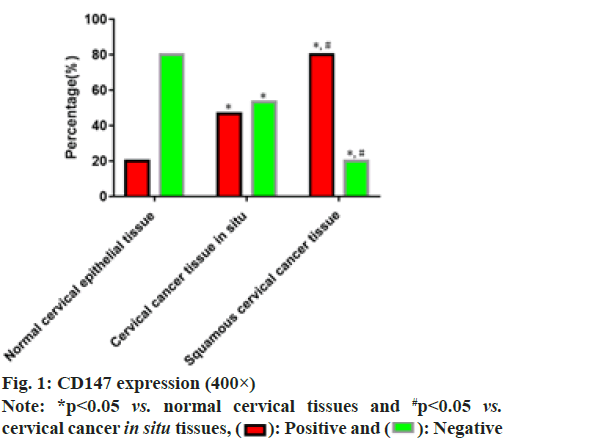
The results of immunohistochemistry indicated that the positive expression rate of CD147 in cervical cancer in situ tissues was significantly increased compared with that in normal cervical tissues, while it was significantly decreased in contrast with that in cervical squamous cell cancer tissues (p<0.05) as shown in fig. 1.
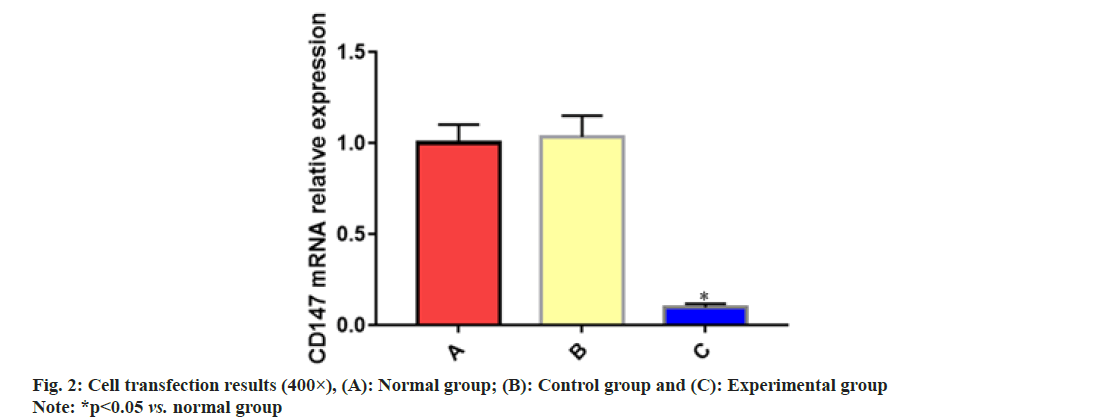
According to the results of correlation analysis, the expression of CD147 was not associated with the age and clinical stage of cervical cancer patients (p>0.05), but had close correlations with the tumor size, invasion depth and lymphatic metastasis in cervical cancer patients (p<0.05) as shown in Table 1. The PCR results manifested that the messenger RNA (mRNA) expression of CD147 was reduced significantly in experimental group in comparison with that in normal group as shown in fig. 2, suggesting that the transfection was successful.
| Item | Quantity n (%) | CD147 | χ2 | p | |
|---|---|---|---|---|---|
| Negative expression | Positive expression | ||||
| Age (year) | 0.004 | 0.95 | |||
| <50 | 42 (46.67) | 12 | 30 | ||
| ≥50 | 48 (53.33) | 14 | 34 | ||
| Tumor size (cm) | 9.097 | 0.003 | |||
| <3 | 50 (55.56) | 10 | 40 | ||
| ≥3 | 40 (44.44) | 16 | 24 | ||
| Clinical stage | 0.163 | 0.686 | |||
| Ia1-Ib1 | 47 (52.22) | 13 | 29 | ||
| Ib2-IIa2 | 43 (47.78) | 13 | 35 | ||
| Invasion depth | 31.15 | <0.001 | |||
| Not into serosa | 45 (50) | 25 | 20 | ||
| Into serosa | 45 (50) | 1 | 44 | ||
| Lymph node metastasis | 18.68 | <0.001 | |||
| No | 44 (48.89) | 22 | 22 | ||
| Yes | 46 (51.11) | 4 | 42 | ||
Table 1: Correlations Cd147 Expression with Clinicopathological Parameters of Cervical Cancer Patients (N=120, %)
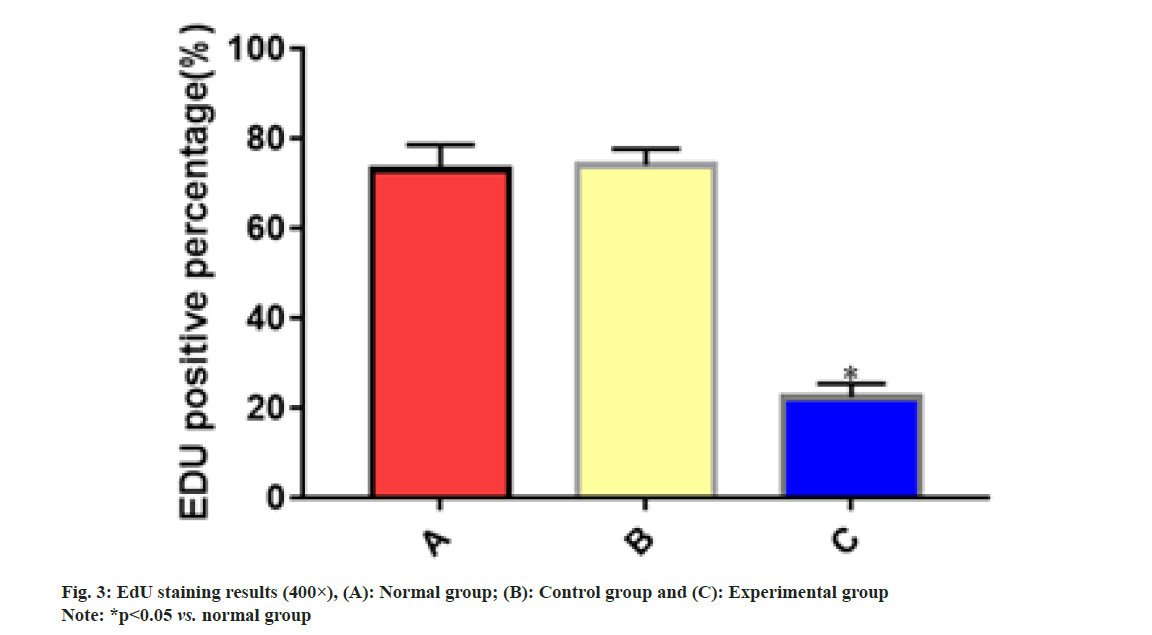
After EdU labeling, the percentage of EdU-positive cells was significantly lower in experimental group than that in normal group (p<0.05). However, there were no significant differences between normal group and control group (p>0.05) as shown in fig. 3.
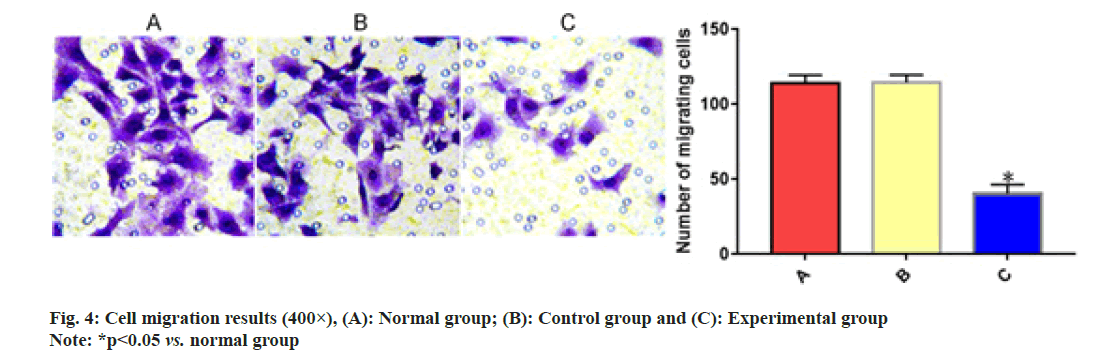
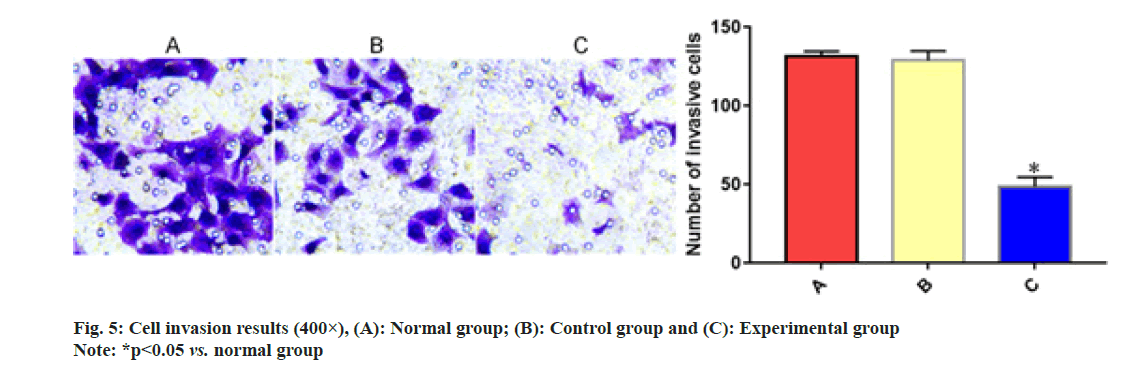
As shown in the results of Transwell assay, experimental group exhibited significantly smaller numbers of migrating cells and cells passing through Matrigel than normal group (p<0.05). However, no significant differences were found between normal group and control group (p>0.05) as shown in fig. 4 and fig. 5.
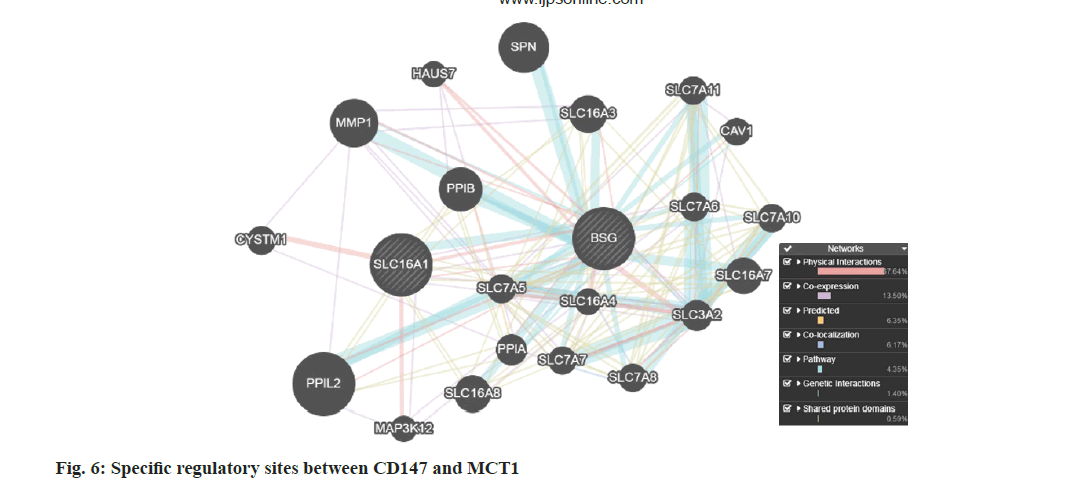
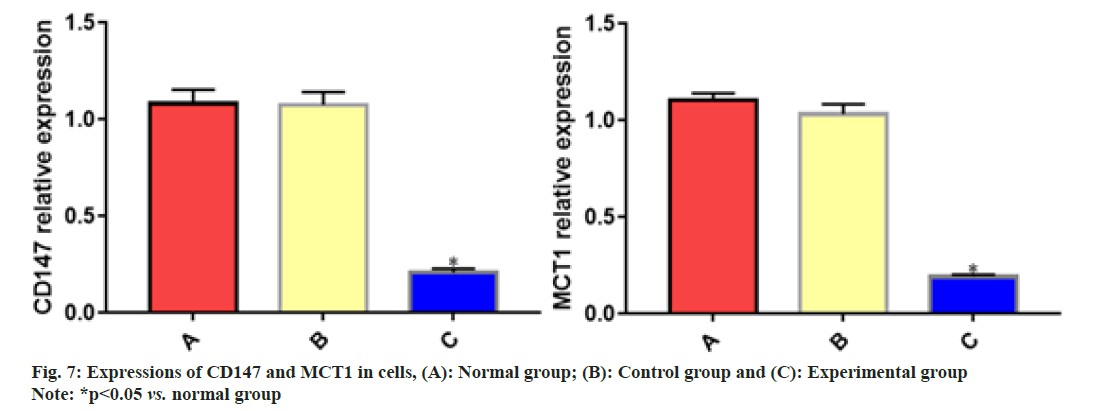
The gene ID of CD147 is Basigin (BSG) and that of MCT1 is Solute Carrier Family 16 Member 1 (SLC16A1). It has been discovered through the GeneMANIA database (http://genemania.org/) that there are specific regulatory sites between CD147 and MCT1 as shown in fig. 6. It was revealed in the results of Western blotting that the protein expressions of CD147 and MCT1 declined significantly in experimental group compared with those in normal group, but they were not significantly different between normal group and control group (p>0.05) as shown in fig. 7. As a common gynecological malignant tumor, cervical cancer frequently occurs in females aged 20-55 y old, seriously threatening the health and life of women worldwide. Although the early screening technique for cervical cancer has been advanced with social development and lifestyle transformation, the age of onset of the disease is becoming younger and younger, and the number of patients who have not given birth to a child is increasing.
In addition, the recurrence and metastasis rates are rising constantly, and the long-term survival rate of the majority of cervical cancer patients is unsatisfying[7]. The molecular mechanism of cervical cancer is very complicated and still under research, so seeking for potential molecular markers for progression of the disease and positively developing efficacious molecular targeted drugs are great challenges faced by clinicians.
CD147 is a type of transmembrane protein of about 58 kD located on the surface of cell membrane, which is expressed in various cells and tissues, such as thymocytes and epithelial cells in human body. Large quantities of studies have demonstrated that CD147 is lowly expressed in normal tissues or cells, but its expression is elevated in many malignant tumors, including urinary system tumor, ovarian cancer, liver cancer and neuroglioma. Therefore, CD147 is a hot spot of research on targeted therapy for malignant tumors. Fang et al.[8] studied and found that the expression of CD147 was increased in prostate cancer and the increased CD147 mediated the Wnt/β-catenin pathway to promote epithelial-mesenchymal transition of tumor cells and disease progression in patients. The study of Min et al.[9] revealed that in the case of renal cell carcinoma, inhibiting the expression elevation of CD147 could remarkably repress the energy metabolism of tumor cells and down-regulate the proliferative ability of cancer cells. Yin et al.[10] denoted that the expression of CD147 rose in esophageal squamous cell carcinoma and the in vitro and in vivo proliferative and invasive abilities of tumor cells were obviously suppressed after the interference of CD147 expression. In the present study, the immunohistochemistry results showed that the expression of CD147 was increased in cervical cancer tissues, accompanied by progression of the disease. Besides, the results of correlation analysis indicated that CD147 expression was highly associated with the tumor size, invasion depth and lymphatic metastasis in cervical cancer patients, suggesting that it is of definite clinical significance to research the expression of CD147 in the case of cervical cancer. Finally, after CD147 expression was silenced by shRNA technique, the cell growth was restrained and the proliferative, invasive and migratory abilities were down-regulated in experimental group, illustrating the potential significance of this target in the clinical treatment of cervical cancer.
The progression of cervical cancer is a slow multistage process involving multiple genes and controlled by various molecules. Specifically, cervical squamous epithelial cells in patients are proliferating abnormally and then activated for differentiation under the stimulation of carcinogenic factors, thereby forming atypical hyperplasia of cervical epithelium (cancer in situ). The synergistic effects of many genes facilitate the disease progression, which gradually develops into squamous intraepithelial lesion, invasive cancer and malignant metastasis to lymph, colon and other target organs, thus endangering patients' lives[11]. MCT1 is a vital mediator for tumor cells to acquire energy through glycolysis. The expression of MCT1 is raised in such tumor tissues as neuroglioma, colon cancer and gastric cancer, and it has a close relationship with the prognosis of patients[12]. Logotheti et al.[13] researched and denoted that inhibiting the expression of MCT1 in bladder cancer could markedly restrain the metabolic reprogramming of tumor cells and the growth of cancer cells. Al-Mousawi et al.[14] reported in study that the down-regulated MCT1 expression in colon cancer HT-29 cells could distinctly reduce the energy needed for tumor cell invasion and malignant metastasis. In this study, it was found in the GeneMANIA database that CD147 and MCT1 had specific regulatory sites. Based on cell experiments, it was discovered that the expression of MCT1 declined evidently in experimental group after silencing CD147 expression.
In conclusion, the expression of CD147 is increased in cervical cancer tissues and repressing CD147 expression can prominently decrease the proliferative, invasive and migratory abilities of tumor cells in vitro and in vivo. However, whether CD147 can be made into a specific probe for the diagnosis of cervical cancer progression needs to be deeply investigated.
Conflict of interests:
The authors declared no conflict of interests.
References
- Dasari S, Wudayagiri R, Valluru L. Cervical cancer: Biomarkers for diagnosis and treatment. Clin Chim Acta 2015;445:7-11.
[Crossref] [Google Scholar] [Pub Med]
- Kremer WW, Steenbergen RD, Heideman DA, Kenter GG, Meijer CJ. The use of host cell DNA methylation analysis in the detection and management of women with advanced cervical intraepithelial neoplasia: A review. BJOG 2021;128(3):504-14.
[Crossref] [Google Scholar] [Pub Med]
- Lu L, Zhang J, Gan P, Wu L, Zhang X. Novel functions of CD147 in the mitochondria exacerbates melanoma metastasis. Int J Biol Sci 2021;17(1):285-97.
[Crossref] [Google Scholar] [Pub Med]
- Suzuki S, Toyoma S, Kawasaki Y, Nanjo H, Yamada T. CD147 promotes invasion and MMP-9 expression through MEK signaling and predicts poor prognosis in hypopharyngeal squamous cell carcinoma. Adv Clin Exp Med 2021;30(1):41-8.
[Crossref] [Google Scholar] [Pub Med]
- Sato N, Saga Y, Uchibori R, Tsukahara T, Urabe M, Kume A, et al. Eradication of cervical cancer in vivo by an AAV vector that encodes shRNA targeting human papillomavirus type 16 E6/E7. Int J Oncol 2018;52(3):687-96.
[Crossref] [Google Scholar] [Pub Med]
- Guo W, Abudumijiti H, Xu L, Hasim A. CD147 promotes cervical cancer migration and invasion by up-regulating fatty acid synthase expression. Int J Clin Exp Pathol 2019;12(12):4280-8.
- Okadome M, Nagayama R, Shimokawa M, Sonoda K, Shimamoto K, Saito T. Prognosis of bulky pTIIB cervical cancer treated by radical hysterectomy comparing adenocarcinoma with squamous cell carcinoma using propensity score matching. Int J Gynecol Obstetr 2021;153(1):56-63.
[Crossref] [Google Scholar] [Pub Med]
- Fang F, Li Q, Wu M, Nie C, Xu H, Wang L. CD147 promotes epithelial?mesenchymal transition of prostate cancer cells via the Wnt/β?catenin pathway. Exp Ther Med 2020;20(4):3154-60.
[Crossref] [Google Scholar] [Pub Med]
- Min X, Zhang X, Li Y, Cao X, Cheng H, Li Y, et al. HSPA12A unstabilizes CD147 to inhibit lactate export and migration in human renal cell carcinoma. Theranostics 2020;10(19):8573-90.
[Crossref] [Google Scholar] [Pub Med]
- Yin Z, Cai H, Wang Z, Jiang Y. Pseudolaric acid B inhibits proliferation, invasion and angiogenesis in esophageal squamous cell carcinoma through regulating CD147. Drug Des Devel Ther 2020;14:4561-73.
[Crossref] [Google Scholar] [Pub Med]
- Hoda N, Rajani BC, Ghosh S, Sabitha KS, Vasantha Dhara B, Nathani J. Cervical lymph node metastasis in squamous cell carcinoma of the buccal mucosa: A retrospective study on pattern of involvement and clinical analysis. Med Oral Patol Oral Cir Bucal 2021;26(1):e84-9.
[Crossref] [Google Scholar] [Pub Med]
- Payen VL, Hsu MY, Rädecke KS, Wyart E, Vazeille T, Bouzin C, et al. Monocarboxylate transporter MCT1 promotes tumor metastasis independently of its activity as a lactate transporter. Cancer Res 2017;77(20):5591-601.
[Crossref] [Google Scholar] [Pub Med]
- Logotheti S, Marquardt S, Gupta SK, Richter C, Edelhäuser BA, Engelmann D, et al. LncRNA-SLC16A1-AS1 induces metabolic reprogramming during bladder cancer progression as target and co-activator of E2F1. Theranostics 2020;10(21):9620-43.
[Crossref] [Google Scholar] [Pub Med]
- Al-Mousawi H, O’Mara M, Stewart G. Identification of the HT-29 cell line as a model for investigating MCT1 transporters in sigmoid colon adenocarcinoma. Biochem Biophys Res Commun 2020;529(2):218-23.
[Crossref] [Google Scholar] [Pub Med]