- *Corresponding Author:
- D. Zhang
Department of Anesthesiology, The People's Hospital of Tongchuan City, Tongchuan City 727000, Shaanxi province, China
E-mail: zhangdz724911158@163.com
| This article was originally published in a special issue, "Clinical and Experimental Studies on Drug and Intervention Repurposing in China |
| Indian J Pharm Sci 2019:81(4)spl issue1;79-85 |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
In order to study the effects of different anesthesia methods on nearest taxon index, mean arterial pressure, heart rate, S-100β protein and other indicators in elderly patients undergoing abdominal surgery, 127 elderly patients hospitalized for abdominal surgery were selected as the study subjects. According to the degree of anesthesia, they were divided into 2 groups one received deep anesthesia and the other shallow anesthesia. The above mentioned indicators were observed in both groups of patients after surgery, to explore the influence of different anesthesia methods on elderly patients. There was no statistical difference in basic information between the two groups, while there was statistical difference in nearest taxon index, mean arterial pressure and heart rate between the two groups (p<0.05). Comparing and analyzing postoperative cognitive dysfunction, postoperative delirium, mini-mental state examination and clock-drawing tests between the two groups, it was found that there was no statistical difference in the comparison of mini mental state exam and CDT scales alone, but the comprehensive comparison between them was more objective and comprehensive, namely post-operative cognitive dysfunction, with statistical difference (p>0.05). In the analysis of serum S-100β protein in two groups, it was found that deep anesthesia not only prevented the increase of S-100β protein, but also quickly restored to the initial level. Therefore, through this study, it is found that different depths of anesthesia has no significant effect on the cognitive function of the elderly, but deep anesthesia has a lower incidence of post-operative cognitive dysfunction than shallow anesthesia and can effectively reduce the level of S-100β protein in patients.
Keywords
Different depths of anaesthesia, the elderly patients, S-100β, quality control
With the progress of society, people's living standards are constantly improving. At the same time, human health has become the focus of attention. As a vulnerable group in society, the elderly often has more emergencies when they are ill; especially when they need surgery, they need to pay more attention to many things[1]. Postoperative delirium (POD) and post-operative cognitive dysfunction (POCD) belong to the category of cognitive decline after surgery, especially after general anaesthesia, which is the most common condition in the elderly. After this condition occurs, patients will need more hospitalization time, higher medical expenses, delayed rehabilitation and lower living standards after surgery. It could lead to complications and death of patients, so it is very important to master the anaesthesia methods and depth of anaesthesia[2,3].
At present, the mechanism of POCD occurrence is not clear. Age is the only definite risk factor for POCD nowadays. A large number of studies show that POCD is closely related to the age of patients and is one of the most common complications of elderly patients after surgery[4]. The occurrence of POCD in elderly patients after abdominal surgery is likely to make the patient's response to various adverse factors weakened and to cause various complications such as abscess, pulmonary hemorrhage and intestinal and gastrointestinal tract infarction[5,6]. Bi-spectral index (BIS) is a more accurate method to monitor the sedation level and depth of anaesthesia by electroencephalogram (EEG). It has been approved by the USFDA for its good correlation with various narcotic drugs[7]. The BIS monitor integrates the phase, frequency and power characteristics of different EEGs into a single variable, and presents them with numbers ranging from 0 to 100. Different numbers represent different anaesthesia depths. By observing the dynamic changes of BIS value, anesthesiologists can predict the depth of anaesthesia and avoid causing too deep or too shallow anaesthesia during operation, which is conducive to the overall control and understanding of the anaesthesia operation process[8,9]. Under BIS monitoring, it is significant to study the effect of different anaesthesia depth on POCD in elderly patients[10]. Up to now, the incidence of POCD is still in the exploratory stage and due to the synergy and interaction of various situations, it is difficult to accurately predict the disease and diagnose it in the clinic. Therefore, this investigation is very essential since it aims to explore the effects of different anaesthesia levels on the physical indicators of the elderly.
In summary, although there are many related studies on POCD, there are still no good methods and means for dealing with the occurrence of POCD in elderly patients. Therefore, 127 elderly patients hospitalized for abdominal surgery were selected as the research subjects, and were divided into two groups according to the degree of anaesthesia, deep anaesthesia and shallow anaesthesia. By observing the relevant indicators in both groups of the patients after surgery, the effect of different anaesthesia levels on elderly patients was explored, with a view to provide new ideas for the treatment of abdominal diseases in the elderly.
In order to better understand the effects of different anaesthesia methods on human related indicators, many researchers have studied its role. Lee et al. studied the effect of anaesthesia in the treatment of bronchial hypertrophy. The results showed that chest computed tomography and fiberoptic bronchoscopy after anaesthesia provided the diagnosis of the airway. If airways are suspected, these examinations are helpful in assessing and managing airways[7]. Bodner et al. studied the perioperative management of patients undergoing thyroidectomy and found that preoperative assessment was helpful to determine the comorbidity and surgical characteristics of patients with increased perioperative risk, and to identify patients with possible airway difficulties[11]; Kreutziger et al. explored the effects of different anaesthesia methods on shoulder pain relief, and the results suggested that whether general anaesthesia, local anaesthesia or intravenous analgesia alone, outpatients can complete shoulder reduction. The clinical results measured by SF-36 and DASH were comparable in the three groups, but the overall operation time was the shortest and patients' satisfaction was higher[12].
Materials and Methods
Research subjects:
One hundred and twenty seven elderly patients hospitalized for abdominal surgery in the First People's Hospital of Tonglu County from February 2014 to April 2019 were selected as subjects. The age ranged from 60 to 80 y, with an average age of 68.7±3.4 y. There were 59 male patients and 68 female patients. According to American Society of Anesthesiologists (ASA) classification I~III, there were 40 ASA grade I patients, 49 ASA grade II patients and 38 ASA grade III patients. Generally, general anaesthesia with tracheal intubation was used during abdominal operation, and the operation time was estimated to be 2-4 h. The study was approved by the Ethics Committee of The First People's Hospital of Tonglu County and informed consent was signed by patients and their families.
Inclusion criteria included age of patients ≥60 y old, according to ASA classification I-III, definite diagnosis and elective laparotomy; no significant history of hypertension, cardiopulmonary disease and related diseases; no serious mental illness; no stroke, brain traumatic disease; no diabetes or impaired glucose tolerance; informed consent signed by patients and their families. Exclusion criteria were long-term neurological and psychiatric disorders, long-term history of sedative and antidepressant drugs; subjects with cardiovascular and liver and kidney impairment; poor compliance behaviour before the study, lack of communication, lack of effective data, and no follow-up after the operation; patients with cognitive impairment suggested by mini mental state exam (MMSE) and clock drawing test (CDT) scores before the study; involuntarily participated subjects.
Grouping:
In the group of 127 elderly patients with abdominal surgery, 3 subjects were withdrawn from the experiment for personal reasons for a period of time. The remaining 124 cases were divided into shallow anaesthesia group (62 cases, low group) and deep anaesthesia group (62 cases, deep group) according to the degree of anaesthesia.
Anaesthesia method:
All patients were fasted for 8 h and had no drinking water for 4 h before operation. No sedative and hypnotic drugs were used before operation. After entering the operating room, patients need to establish a routine venous channel. ECG, respiratory rate and pulse oxygen saturation were monitored by ECG monitor. Connect BIS Vista EEG monitor to monitor nearest taxon index (NTI), routinely disinfect patients' forehead skin, use special coupling agent, and place electrode slice. NT monitor uses single channel, and electrode resistance <6KΩ. Make conventional mask oxygen inhalation (6 l/min). Radial artery catheterization was conducted under local anaesthesia, invasive blood pressure was monitored, right internal jugular vein was catheterized, depth of 12 to 15 cm, and central venous pressure was monitored.
Then, anaesthesia was induced. Firstly, midazolam (0.05 mg/kg) was injected intravenously, then propofol (3 mg/kg·h) was infused by intravenous pump. The concentration was increased by 0.5 mg/kg every 2 min. Intraoperative anaesthesia depth NTI for different groups reached the corresponding standard (low group were controlled at 47-63, deep group were controlled at 20-35), then fentanyl (2-3 g/kg) and rocuronium (0.6 mg/kg) were injected intravenously, tracheal intubation (propofol concentration during intubation was regulated by a dedicated person) and mechanical ventilation (setting) were performed on the anaesthesia machine (respiratory parametersoxygen flow rate 2 l/min, tidal volume 8-10 ml/kg, respiratory frequency 11-13 times/min, respiratory ratio 1:2). Anaesthesia was maintained during surgery using a propofol intravenous pump (1-5 mg/kg·h) and remifentanil (0.05~0.2 μg/kg·min). Both groups were given the same anaesthesia (fentanyl l 6 μg/kg+saline 100 ml, intravenous injection, speed 2 ml/h).
Observation indicators:
The baseline data such as age, gender, anaesthesia time and operation time were recorded, and the occurrence and duration of POD were also recorded. One day before operation (16:00-20:00), one day after operation, and three days after operation (2 times a day, 6:00-8:00 and 18:00-20:00), were assessed by two follow-up patients trained by professional psychiatrists using the confusion assessment method (CAM). Visual analogue scale (VAS) scores were recorded and pain was assessed 24 h after operation, i.e. one day after operation. The data of NTI, mean arterial pressure (MAP) and heart rate (HR) before induction (T0), after induction (T1), after intubation (T2), after operation (T3), 1 h in the operation (T4), 2 h in the operation (T5), after the operation completed (T6), after extubation (T7) were recorded. The MMSE score and CDT score of the patients 1 d before induction (a), 24 h after operation (b) and 3 d after operation (c) were recorded and assessed; S-100β protein data of patients were recorded and compared. The S-100β protein detection kit established a rapid, specific and simple quantitative detection established by using immunochromatographic technology and interpreted by immune-quantitative analyser.
The results were assessed before induction (T0), 2 h in the operation (T5), after the operation completed (T6), after extubation (T7) and 24 h after operation (b). The data were analysed by repeated variance analysis. Postoperative cognitive impairment was analysed by international POCD composite Z-score method.
Evaluation criterion:
Delirium was assessed by the CAM on day 1 before operation and the d 3 after operation[13], which included four aspects, 1. the course of acute attack and fluctuation; 2. inattention; 3. incoherence of thinking and 4. change of consciousness. Delirium can be diagnosed with one of 1 and 2 or 3 or 4.
VAS score- pain degree was divided into 0 to 10 points, 0 points for no pain, 10 points for severe pain, increasing in turn, respectively, indicating increased pain. Guide the patient to choose the corresponding score according to the actual pain situation, record the pain score after the operation. 0-2 points indicated good analgesia, 3-4 points indicated reliable analgesia, and ≥4 points indicated incomplete analgesia[14]. MMSE scale- score <17 indicated illiteracy (uneducated level), 17≤ score <20 indicated primary school education (education ≤6 y), education >6 y, and score <24 indicated cognitive impairment[15].
CDT score- patients were required to draw a clock disc on an A4 paper in an independent environment, and mark the correct needle at the designated time and position, and then evaluated by quartile method. 1 point- drew a closed circle; 2 points- drew a closed circle and put the number in the right place; 3 pointsdrew a closed circle, and the number is correct, including 12 positions and the correct order and 4 points- put the pointer in the right place[16].
POCD criteria- according to MMSE score and CDT score, the occurrence of POCD was judged by the reduction of post-operative score and pre-operative score of MMSE ≥2, and the decrease of post-operative score and pre-operative score ≥1[17].
Quality control method:
Double blind method was used to investigate and record the data. Investigators were trained in POD, POCD, MMSE, VAS, CDT and other assessment tools. If they could use them independently and correctly, they could start the investigation. Before the investigation, the investigators gave a brief description of the survey tools for patients, including content, method, role, and so on. They made a preliminary investigation for patients. After the preliminary investigation, they began to investigate. The survey was conducted by two persons, one person was responsible for introducing the survey tools and describing the methods, and the another person was responsible for recording the survey data. The survey was completed after both persons confirmed that the survey data were correct. In the course of investigation, patients needed not be disturbed by external factors and should complete it independently.
Statistical methods:
Epidata3.1 software was used to establish the database. All data were entered by two persons and two copies. Logical verification and spot check were carried out. If the qualified rate of spot check was above 96 %, the data was considered valid. The effective data were analysed by SPSS22.0 software. The descriptive analysis was used to analyse the patient's measurement data. The homogeneity of variance was analysed by t-test, and the counting data by x2-test. The results showed that there was statistical significance with p<0.05 showed significant difference.
Results and Discussion
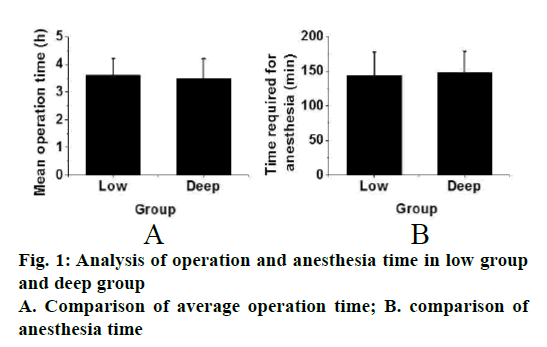
From Table 1, the basic information of the two groups can be obtained, including the proportion of male and female, average age, average height, average weight, type of operation, ASA classification, average operation time and anaesthesia time. There was no statistical difference between the two groups (p>0.05, fig. 1).
| Cases | Low Group | Deep Group |
|---|---|---|
| 62 | 62 | |
| Proportion of male to female | 37/25 | 36/26 |
| Average age (y) | 69.8±4.1 | 68.2±3.9 |
| Average height (cm) | 167.3±8.1 | 168.2±6.9 |
| Average weight (kg) | 61.5±3.7 | 63.2±3.3 |
| Type of operation (stomach/intestine) | 32/30 | 36/26 |
| ASA classification (I/II/III) | 21/25/16 | 19/23/20 |
| Average operation time (H) | 3.6±0.6 | 3.5±0.7 |
| Anesthesia time (min) | 143.5±34.1 | 147.6±31.2 |
Table 1: General data analysis of low group and deep group
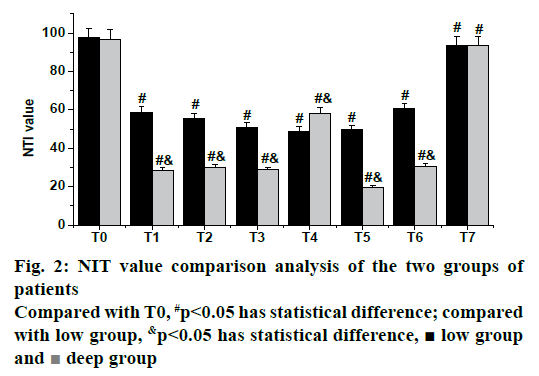
Fig. 2 shows the results of NIT index comparison between the two groups. There were significant differences in T1 (after induction), T2 (after intubation), T3 (after operation), T4 (1 h during operation), T5 (2 h during operation), T6 (after the operation completed), T7 (after extubation), and T0 (before induction) between the low group and the deep group (p<0.05). There were statistical differences between the two groups in data of T1, T2, T3, T4, T5 and T6, respectively (p<0.05), but there was no statistical difference between the two groups in NTI values of T7 and T0 (p>0.05).
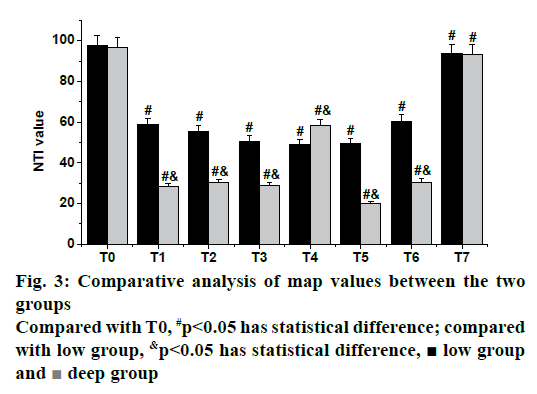
As shown in fig. 3, the results of MAP in both groups showed that there were significant differences in T1 and T2 between low group and deep group compared with T0 (p<0.05), while there was no significant difference in other data of the deep group compared with the low group (p>0.05).
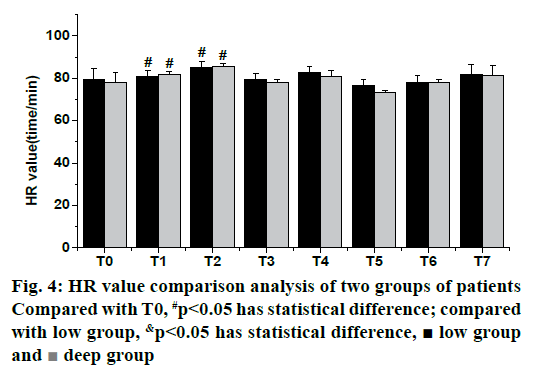
As shown in fig. 4, the HR values of the two groups were compared. It was found that there were significant differences in T1, T2 and T0 between the low group and the deep group (p<0.05), while there was no significant difference in other data of the deep group compared with the low group (p>0.05).
As shown in Table 2, the intraoperative condition, anesthetic dose and VAS score of the two groups were compared and analysed. It can be found from the table that the dosage of anaesthetics used in the deep group was higher than that in the low group (p<0.05), and there was no statistical difference in VAS scores during and after operation between the two groups (p>0.05). Therefore, there was no significant difference between the deep group and the low group in VAS scores during and after operation, except for the dose of anaesthetics.
| Low group | Deep group | |
|---|---|---|
| Intraoperative blood loss (ml) | 362.4±50.1 | 387.1±52.1 |
| Intraoperative fluid infusion volume (ml) | 1861.2±291.5 | 2034.1±273.2 |
| Midazolam (mg) | 2.7±1.2 | 3.0±1.4 |
| Propofol (mg) | 941.2±51.3 | 1076.5±53.7 |
| Fentanyl (mg) | 0.53±0.2 | 0.61±0.3 |
| Remifentanil (mg) | 3.1±1.1 | 3.2±0.9 |
| VAS score | 2.2±0.6 | 1.8±0.8 |
Table 2: Comparison of intraoperative condition, anesthesia dose and VAS score between low group and deep group
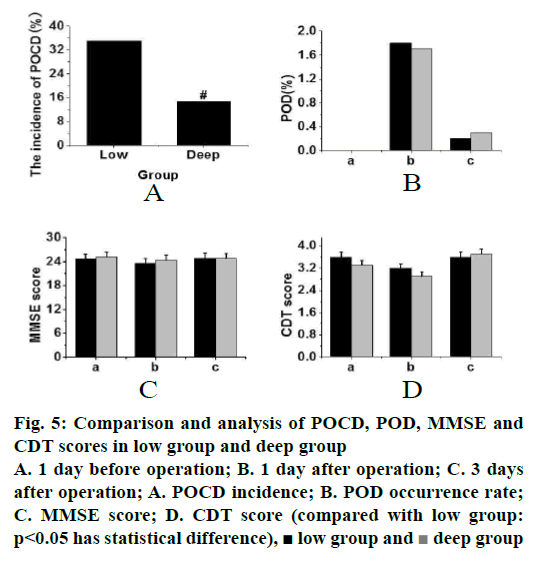
The POCD, POD, MMSE and CDT scores of the low group and the deep group were compared and analysed, and the data were recorded (fig. 5). As shown in fig. 5A, the incidence of POCD in the deep group was lower than that in the low group (p<0.05). From fig. 5B, it was found that there was no significant difference in POD between the deep group and the low group (p>0.05). From fig. 5C, it can be concluded that the difference in MMSE score between the low group and the deep group was small and there was no significant difference. From the CDT score of fig. 5D, it was found that the change trend of the low group was the same as that of the deep group, and there was no significant difference. Therefore, it can be concluded that no significant difference between the two groups if the MMSE and CDT scores were observed alone, but after combining the two scales, it was found that there were significant differences between the two groups, which could make the evaluation more comprehensive and the conclusions more objective.
Figure 5: Comparison and analysis of POCD, POD, MMSE and CDT scores in low group and deep group
A. 1 day before operation; B. 1 day after operation; C. 3 days
after operation; A. POCD incidence; B. POD occurrence rate;
C. MMSE score; D. CDT score (compared with low group:
p<0.05 has statistical difference),  low group and
low group and  deep group
deep group
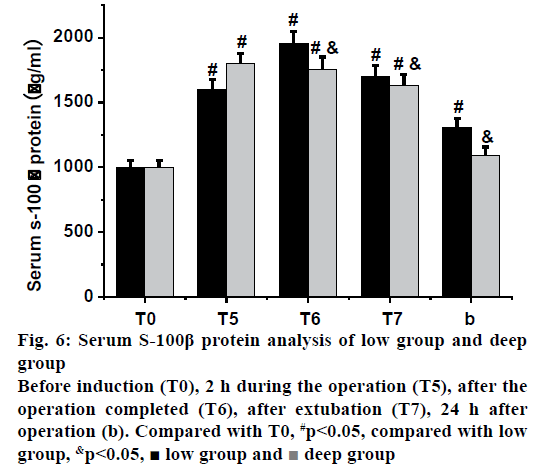
As shown in fig. 6, the serum S-100β protein levels in the low group and the deep group were compared and analysed. It was found that there were significant differences between the 2 h during the operation, after the operation completed, 2 h after operation and 24 h after operation in the low and before induction (p<0.05); after the operation completed, 2 h after operation, and 24 h after operation of the low group were lower than those of the deep group, respectively, and there was statistical significance (p<0.05). Therefore, it can be inferred that deep anaesthesia can effectively reduce the increase of S-100β protein level in elderly patients, and recover to normal level in a period of time after operation, which indicated that deep anaesthesia can protect the nerves of elderly patients during operation.
In order to study the effects of different anaesthesia methods on NTI index, MAP, HR, S-100β protein and other indicators in elderly patients undergoing abdominal surgery, 127 elderly patients hospitalized for abdominal surgery were selected as the research subjects. According to the degree of anaesthesia, they were divided into the deep group and the low group. The effect of different anaesthesia methods on elderly patients was explored by observing the related indicators in the two groups of patients after surgery. There was no significant difference in basic information between the two groups (p>0.05) but there were significant differences in NIT, MAP and HR between the two groups (p<0.05). Comparing and analysing POCD, POD, MMSE, and CDT between the two groups, it was found that there was no significant difference in the comparison of MMSE and CDT scales alone, but combining both resulted in a more objective and comprehensive comparison, namely POCD, with statistical difference (p>0.05). In the analysis of serum S-100β protein in two groups, it was found that the deep anaesthesia not only prevented the increase of S-100β protein, but also quickly restored it to the initial level.
In conclusion, by exploring the relationship between different anaesthesia modes and various indicators of elderly patients, it is found that different depths of anaesthesia has no significant effect on postoperative cognitive function of elderly patients, but the deep group has lower incidence of POCD and can effectively reduce the S-100β protein level of patients compared with the low group, which provides experimental data for surgical treatment of elderly patients. However, there were still some deficiencies in this study, such as the small sample size in the experimental process, unable to accurately explore its mechanism. Therefore, it is necessary to increase the sample size to further explore the mechanism.
References
- Zhang XK, Hu Q, Chen QH, Wang WX. The effect of continuous perfusion of esmolol on cardiovascular risk in elderly patients undergoing noncardiac surgery. Pharmazie 2017;72(8):487-489.
- Wang LH, Zhu RF, Gao C, Wang SL, Shen LZ. Application of enhanced recovery after gastric cancer surgery: An updated meta-analysis. World J Gastroenterol 2018;24(14):1562.
- Ranum D, Beverly A, Shapiro FE, Urman RD. Leading Causes of Anesthesia-Related Liability Claims in Ambulatory Surgery Centers. J Patient Saf 2017;16:1.
- Farmer L, Winfield C, Quatrara B, Letzkus L, Schenck P, Finneran P. Does Site Matter? Comparing Accuracy and Patient Comfort of Blood Glucose Samples Taken from the Finger and Palm of the Perioperative Patient. J Perianesth Nurs 2017; 32(6):573-7.
- Epstein RH, Dexter F, Gratch DM, Lubarsky DA. Intraoperative Handoffs Among Anesthesia Providers Increase the Incidence of Documentation Errors for Controlled Drugs. Jt Comm J Qual Patient Saf 2017;43(8):396.
- Tulgar S, Thomas DT, Deveci U. Erector spinae plane block provides sufficient surgical anesthesia for ileostomy closure in a high-risk patient. J Clin Anesth 2018;48:2-3.
- Lee CC, Lin BS, Chen JY, Chuang CC. Anesthesia for a patient with unexpected giant tracheobronchomegaly. Ci Ji Yi Xue Za Zhi 2017;29(1):59-61.
- Chang B, Kaye AD, Diaz JH, Westlake B, Dutton RP, Urman RD. Interventional Procedures Outside of the Operating Room: Results from the National Anesthesia Clinical Outcomes Registry. J Patient Saf 2018;14:9-16.
- Mcdonald H. Anaesthesia for the Elderly Patient. Canadian J Anesth 2017;64(10):1082-1083.
- Çakar E, Yilmaz E, Çakar E, Baydur H. The Effect of Preoperative Oral Carbohydrate Solution Intake on Patient Comfort: A Randomized Controlled Study. J Perianesth Nurs 2017; 32(6):589.
- Bodner GB, Talbott AL. Preanesthesia concerns in a patient with a thyroid mass. JAAPA 2018; 31(3):1-3.
- Kreutziger J, Hirschi D, Fischer S, Herzog RF, Zbinden S, Honigmann P. Comparison of interscalene block, general anesthesia, and intravenous analgesia for out-patient shoulder reduction. J Anesth 2019; 33(2):1-8.
- Hernandez BA, Lindroth H, Rowley P, Boncyk C, Raz A, Gaskell A, et al. Post-anaesthesia care unit delirium: incidence, risk factors and associated adverse outcomes. Br J Anaesth 2017;119(2):288-90.
- Fu M, Li D. General anesthesia combined with epidural anesthesia on the postoperative cognitive functions in pregnant women with dystocia. Exp Ther Med 2018;16(2):1149-52.
- Qian S, Jian P, Yuan S. Effects of remifentanil combined with propofol anesthesia on IL-1β, IL-6, TNF-α and hemodynamics in patients with brain surgery. J Hainan Med Univ 2017;23(15):61.
- Haghighi M, Sedighinejad A, Nabi BN, Mardani-Kivi M, Tehran SG, Mirfazli SA, et al. Is Spinal Anesthesia with Low Dose Lidocaine Better than Sevoflorane Anesthesia in Patients Undergoing Hip Fracture Surgery. Arch Bone Jt Surg 2017;5(4):226.
- Hanbeyoglu O, Urfalioglu A, Yazar FM. Effects on QTc Interval of 2 Different Doses of Spinal Anesthesia in Inguinal Hernia Operations. Med Sci Monit 2017;23:1261-7.