- *Corresponding Author:
- Jian An. Li
Center of Rehabilitation Medicine, The First Affiliated Hospital of Nanjing Medical University, Nanjing, China;
E-mail: lijianan@njmu.edu.cn
| This article was originally published in a special issue, “Biomedical Research in Clinical and Preclinical Pharmaceutics” |
| Indian J Pharm Sci 2020:82(5) Spl issue7;102-109 |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
To investigate the effects of early active motion versus early passive motion on functional recovery of repaired flexor digitorum tendon in Zone-II, and the feasibility of shear wave elastography in monitoring the tension of flexor tendons. Thirty-six patients were randomly divided into early active motion (n=18) and early passive motion (n=18) groups for accordingly treatments. Before treatment, Young’s modulus of flexor tendon was measured with shear wave elastography. The total active motion was evaluated at 4, 8, 12, and 16 w post-operation. At 16 w; grip strength, pinch strength, adjusted Strickland’s classification and the disabilities of the arm, shoulder and hand score were assessed. At a 16-w follow-up, the total active motion (215.48±22.75°) and grip strength (21.07±5.84 kg) of the early active motion group was significantly higher than those (191.00±33.15° and 15.75±7.91 kg) early passive motion group (p<0.05). The repeated measurement method of the general linear model of total active motion showed that treatment protocol, time, and the interaction between two elements had significant effects on the functional results. According to the adjusted Strickland’s system, the good and excellent recovery rate was 100 % in the early active motion group and 76.1 % in the early passive motion group. Early active mobilization had better tendon gliding and excursion even with the two-strand repair as active motion will decrease adhesion formation, with significant difference compared with the passive group. No significant differences between these two groups were found in the pinch force and disabilities of the arm, shoulder and hand score. Young’s Modulus in active finger flexion was significantly higher than that of immobilization position, and it was lowest in passive flexion status (p<0.05). Early active motion contributes to better joint mobility and grip strength after Zone-II flexor tendon repaired. Application of shear wave elastography in monitoring flexor tendon tension appears feasible.
Keywords
Early active motion (EAM); Digital flexor tendon; Total active motion (TAM)
Over the last 50 y, the rehabilitation of patients after surgical repair of the digital flexor tendon in zone II has been evolving in an increasingly aggressive direction with the advancements in surgical techniques and equipment[1]. The post-operational rehabilitation protocol has evolved from complete immobilization to passive motion[2], place-and-hold[3] and synergistic motion[4], till recently proposed the Manchester short orthosis[5], and Saint John protocol[6]. However, there has been little agreement on exercise mode for repaired flexor tendon so far. Tang[1,7] promoted the early true active finger flexion through instructing patients after 4-strand or 6-strand core suture repairs to flex fingers up to half of the full flexion range. Yet, a retrospective analysis that compared studies with early active versus passive exercise found no statistical difference of total active motion (TAM) in the trials with 12 w followup[8]. There was a randomized controlled trial (RCT) showed that the place-and-hold exercises provided better outcomes than a passive motion for patients with flexor tendon repaired in zone II[9]. In a place-and-hold session, the affected digits were passively flexed by unaffected hand, and then the patients were instructed to maintain the clenched fist by active contraction of the involved muscles[9]. Technically, the place-andhold exercise was not the true active motion of the affected hands. The controversy of previous studies might explain the reason why the conservative passive mobilization regimens were still popular in real clinical practice to date. There is an urgent need to address an RCT investigation on the efficacy and safety of the truly early active motion protocol[10].
Another reason for the popularity of conservative regimens could be attributed to the lack of methods to detect real-time tendon tension, which hindered the promotion of early active motion protocol due to safety concerns. Shear wave elastography (SWE), a quantitative and non-invasive technique, has been validated to estimate dynamic changes of tendon’s elasticity in real-time[11,12]. It can indirectly reflect instantaneous changes in the tension of the Achilles tendon under different tensile loads or in different positions[13,14]. However, no data upto date has been reported in its application in the flexor digitorum profundus (FDP) tendon. The attempt using SWE to measure the stiffness of the flexor tendon might provide a new method to monitor the tension generated on the tendon inside the wound. In this study, a randomized controlled trial was performed to compare the efficacy and safety of early active motion and passive motion in patients after surgical repair of Zone-II flexor tendons. Meanwhile, the elasticity of the FDP tendon was estimated under different immobilization positions and motion status using the SWE technique, to explore the feasibility of SWE in monitoring the tension of flexor tendons.
Materials and Methods
Study design and participants:
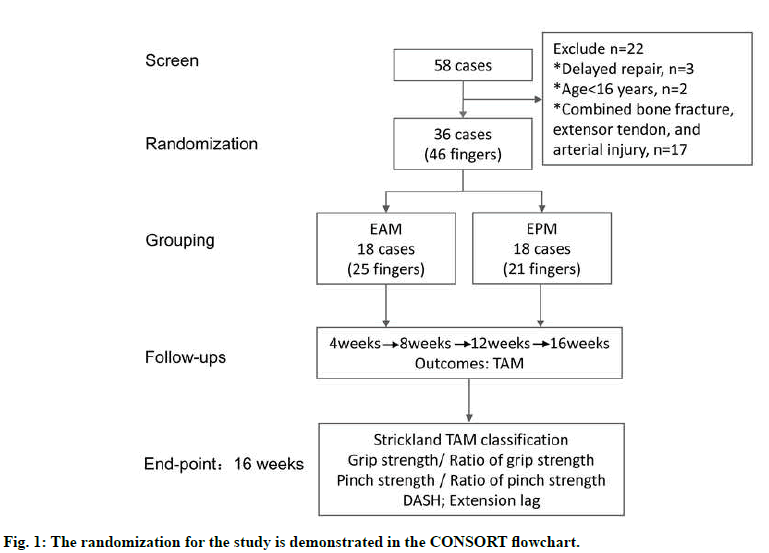
The present study was a prospective parallel assessorblinded randomized control trial to examine the effects of early active motion (EAM) versus early passive motion (EPM) on functional recovery after digital flexor tendon repair in zone II. The ethics committee of Wuxi 9th Affiliated Hospital of Soochow University approved this study (Study number: KT2019002), and the trial was registered at the Chinese clinical trial registry (http://www.chictr.org.cn/index.aspx) with the unique identifier ChiCTR2000030592. From February to December 2019, patients who underwent surgically repair for Zone-II flexor tendon rupture using 4-strand modified Kessler core suture combined with epitendinous suture were enrolled in this study[15]. They were randomized into two groups after surgery but before beginning therapy, as demonstrated in the CONSORT (Consolidated Standards of Reporting Trials) (fig. 1). The random allocation sequence was generated using the Excel RAND function. Then research coordinator performed the randomization by allocating patients into the EAM or EPM group based on the sequence. Written informed consent was obtained from each patient at the same time. Treatments were performed by two therapists, each with more than three y of experience in hand therapy. Two physicians from the rehabilitation department performed the followup process. Therapists and physicians were trained separately before the trial to ensure the consistency of treatment and evaluation. The SWE measurements were performed by a sonographer with more than five y experience.
Inclusion and exclusion criteria:
Patients were considered eligible if they were: aged between 16 and 75 y; post-operational with complete laceration of Zone-II flexor digitorum profundus (FDP) tendon, with or without laceration of flexor digitorum superficialis (FDS) tendon; eligible for end-to-end repair because of minimal deficit of the tendons; in compliance with regular outpatient visits and followups; willing to sign the informed consent and participate in the trial. Cases with the following conditions were excluded: tendon injury located outside of the zone-II area; finger crush injuries with bone fracture, extensor tendon, and arterial injury, or other injuries of the same upper limb; delayed repairs over two w; cases requiring tendon transplantation or suture with high tension due to defection of repaired tendon; congenital dysplasia or deformity of the injured hand; mental illness or poor compliance.
Sample size calculation:
The sample size was estimated based on a twosample independent t-test, using the freeware program G*Power, version 3.1. The effect size was calculated to be 1.19, according to the results of Trumble’s research[16]. At least 28 cases were required to reach a statistical power of 90 % under the circumstance of a significant threshold being p=0.05. With 20 % of the dropout rate taken into account, the minimal sample size was 35 cases.
Demographic data:
A total of 58 patients were screened during the study period, and 36 patients met the inclusion criteria and were enrolled. Eighteen patients (25 fingers) were enrolled in the EAM group, and eighteen patients (21 fingers) were enrolled in the EPM group. Each patients were treated in out-patients’ clinic twice a w for 16 consecutive w according to pre-fabricated protocols. No patients dropped out at 16 w follow-up. The average age of the patients was 38.7±12.8 y, ranging between 17 and 72 y. There were 23 male patients and 13 female patients. Twenty four patients had injuries involving the dominant hand. No significant demographic differences were found between the groups (age, sex, education level, injured fingers, and hand dominance).
EAM and EPM protocols:
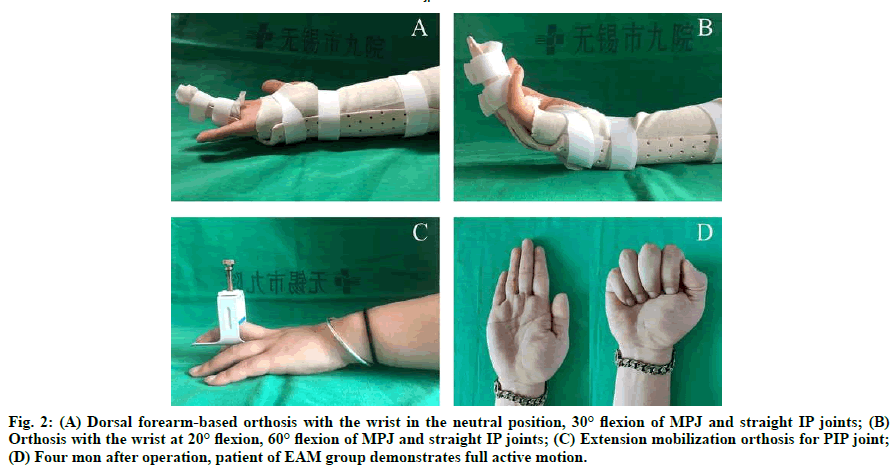
In the EAM protocol, the plaster was replaced by a thermoplastic dorsal forearm-based orthosis to fix the wrist in the neutral position, 30° flexion of metacarpophalangeal (MP) joint, and straight interphalangeal (IP) joint in 3 to 5 d after surgery (fig. 2A). The patients were instructed to perform a set of sequential movements: passive flexion of the MP and IP joints to the fist position, and subsequent active extension of the fingers to the orthosis limit position; partial active finger flexion: gently flex fingers within half of the range of motion, and stop when encountering resistance; anti-blocking exercise: extension of the IP joint to the neutral position while keeping the MP joint flexed; a circular movement of the wrist joint while maintaining a passive fist. The orthosis would be removed during exercise, which was performed 30 repetitions per set, 4 sets each d. After 2 w, patients began to do slight active finger flexion beyond the first 1/2 range of motion under the therapist’s supervision.
Fig. 2: (A) Dorsal forearm-based orthosis with the wrist in the neutral position, 30° flexion of MPJ and straight IP joints; (B) Orthosis with the wrist at 20° flexion, 60° flexion of MPJ and straight IP joints; (C) Extension mobilization orthosis for PIP joint; (D) Four mon after operation, patient of EAM group demonstrates full active motion.
In the EPM protocol, the wrist was fixed at 20° flexion, the MP joint at 60° flexion, and the IP joint at 0° using the orthosis (fig. 2B). The patients were prescribed with passive exercises within 3 to 5 d after the operation, including: keeping the MP joint at 90° flexion, and doing passive flexion and active extension of the distal and the proximal IP joint respectively; passive flexion of all fingers to full-fist position and subsequent active digital extension in orthosis.
Patients from both groups were instructed to elevate the affected limb, while the retrospective massage and compression wrap (Coban, 3M, Minnesota, USA) were applied to control swelling. When the suture was removed two w after surgery, the hand therapist initiated the instruction of scar treatment. After four w, all patients in both groups were allowed to perform light active flexion exercise and active wrist exercises. Progressive resistance exercises and blocking exercises were allowed after six to eight w. If patients had extension lag in their PIP joints, an extra extension mobilization orthosis was used at night (fig. 2C). In the 10th w, the daily use of the injured hand was allowed for light works, and heavy works started after 12 w (fig. 2D).
Outcomes:
The total active motion (TAM) was measured using a Jamar™ goniometer at 4, 8, 12, and 16 w after surgery. The flexion and extension angles of the distal/proximal IP (DIP / PIP) and MP joints were measured at the active grip and finger extension positions, respectively. TAM was calculated with the following formula: TAM=total digital flexion (MP+PIP+DIP)-total digital extension lag (MP+PIP+DIP).
Based on the overall active range of motion (AROM) of the PIP and DIP joints, the proportion of fingers achieved excellent or good grade was calculated according to the adjusted Strickland’s system, and extension lag of PIP joint was observed and recorded for each finger. At 16 w after surgery, the grip strength was measured using the Jamar™ dynamometer, while the patient was seated with his/her shoulder adducted, elbow flexed at 90°, and forearm in a neutral position. Meanwhile, the tip pinch was measured using the Jamar™ pinch gauge. The percentage of the grip or pinch strength on the contralateral side was calculated to eliminate the effect of individual differences. The patients were requested to fill out the validated Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire at 16 w after surgery[17]. The DASH score is a thirtyquestion survey that evaluates symptoms and function in patients with up-extremity disorders, with scores ranging from 0 (normal) to 100 (completely disabled)[18].
Shear wave elastography measurement:
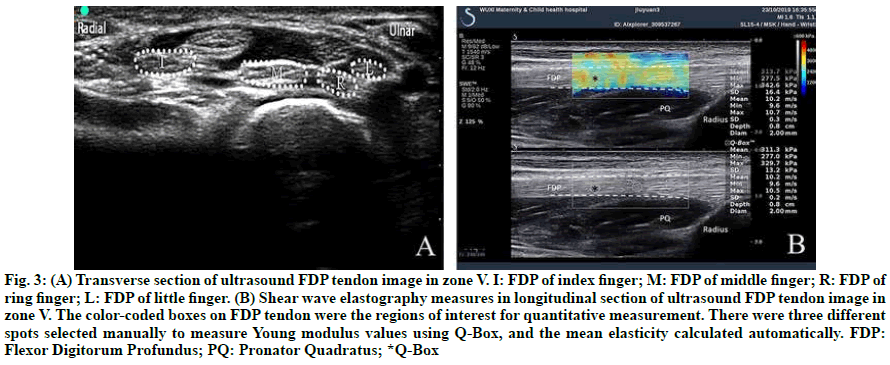
On the first d of the post-operational intervention, Young’s modulus of flexor tendon[13] was measured using Supersonic Aixplorer system (Supersonic Imagine, Aixen- Provence, France)[14] with a 4 to 15 MHz frequency linear array probe to explore the feasibility of the SWE technique in detecting the tension of FDP tendons. The patient took a sitting position, placed the affected hand on an orthosis with the palm facing upwards, the elbow flexed and the forearm supinated. After identifying the target flexor tendon on the transversal section in zone V (fig. 3A), the sonographer switched the probe to the longitudinal section of the tendon. When obtained a stable and clear image of the target flexor tendon, the system was guided to a shear wave elastography procedure, and the sampling frame was located to cover the upper and lower boundaries of the tendon. The Q-BOX with a diameter of 2 mm was placed on the left, middle and right part of the flexor tendon in the sampling frame in order (fig. 3B). The Aixplorer system automatically calculated the average Young’s modulus. The methods as mentioned above were used to measure Young’s modulus of the target flexor tendons at the following positions: orthosis-immobilized position; active finger flexion position (EAM group) and passive full-fist position (EPM group).
Fig. 3: (A) Transverse section of ultrasound FDP tendon image in zone V. I: FDP of index finger; M: FDP of middle finger; R: FDP of ring finger; L: FDP of little finger. (B) Shear wave elastography measures in longitudinal section of ultrasound FDP tendon image in zone V. The color-coded boxes on FDP tendon were the regions of interest for quantitative measurement. There were three different spots selected manually to measure Young modulus values using Q-Box, and the mean elasticity calculated automatically. FDP: Flexor Digitorum Profundus; PQ: Pronator Quadratus; *Q-Box
Statistical analysis:
All statistical analyses were performed using the SPSS 22.0 software (IBM Corporation). For the functional parameters (TAM, grip strength ratio, pinch strength ratio, and DASH score) at 16 w after surgery, normal tests and homogeneity tests of variance were performed before independent t-tests. The functional grading by adjusted Strickland’s system of the two groups was tested using a cross-tab chi-square test. Repeated analysis of variance was performed for TAM at 4, 8, 12, and 16 w after the operation. The follow-up time was considered as an intra-group factor, and different treatments were analyzed as inter-group factors. The F value and p value of the Roy’s Largest Root test[19] in the multivariate test were directly adopted as the result if the data were consistent with Mauchly’s test of sphericity[20], otherwise, the values were corrected by the Greenhouse-Geisser method[21]. The Young’s modulus of FDP tendon was collected in orthosis-fixed position and active/passive finger flexion status, respectively. Data were expressed as mean±standard deviation (SD). Differences in Young’s modulus of flexor tendons between groups in orthosis-fixed position and finger flexion status were compared using independent sample t-test. p<0.05 was considered statistically significant.
Results and Discussion
At the 16 w follow-up, there were no adverse events or secondary lacerations. As shown in TABLE 1, there was no significant difference in TAM recovery between the two groups at four w post-operation. At 8, 12, 16 w, the TAM recovery of the EAM group was significantly higher than the EPM group. Both groups had extension lag in the PIP joint, with two cases in the EAM group and three cases in the EPM group. The adjusted Strickland’s system was used to categorize the recovery of affected finger function based on the range of motion of distal and proximal IP joints. The excellent rates are 100 % in the EAM group and 76.1 % in the EPM group. The grip strength, pinch strength, and DASH of the EAM group were higher than those of the EPM group, but only the grip strength (grip strength ratio) was statistically significant between groups (TABLE 2).
| n* | Times | EAM (n=25) | EPM (n=21) | p-value |
|---|---|---|---|---|
| TAM (°) | 4w | 177.68±19.28 | 163.81±28.06 | 0.054 |
| 8w | 191.24±19.51 | 172.86±29.52 | 0.015* | |
| 12w | 202.48±20.58 | 181.95±31.27 | 0.011* | |
| 16w | 215.48±22.75 | 191.00±33.15 | 0.005** |
*n: number of fingers; p<0.01;*p<0.05.
Table 1: A Comparison of Tam Between the Eam and Epm Groups at Multiple Follow-Ups
| EAM (n=18) | EPM (n=18) | p-value | |
|---|---|---|---|
| Grip strength (kg) | 21.07±5.84 | 15.75±7.91 | 0.028* |
| Ratio of grip strength (%) | 78.33±19.63 | 60.89±24.71 | 0.025* |
| Pinch strength (kg) | 7.95±3.40 | 7.38±3.94 | 0.647 |
| Ratio of pinch strength (%) | 69.94±19.76 | 63.17±25.38 | 0.378 |
| DASH | 3.20±1.98 | 4.44±2.17 | 0.081 |
| Extension Lag | 2 (8 %) | 3 (19 %) | 0.266 |
| Adjusted Strickland’s system | |||
| Excellent | 10 (40 %) | 4 (19 %) | 0.013* (c2 for trend) |
| Good | 15 (60 %) | 12 (57.1 %) | |
| Fair | 0 (0 %) | 4 (19 %) | |
| Poor | 0 (0 %) | 1 (4.9 %) | |
**p<0.01; *p<0.05.
Table 2: Functional Parameters in the Eam and Epm Groups at 16 W
Patients in both groups were measured for TAM at fourtime points: 4 w, 8 w, 12 w, and 16 w after surgery. Data were tested using a general linear model of repeated measurement design. The time factor was four-time points, and the treatment program referred to EAM and EPM. The results showed that both the time factor and the treatment program affected the treatment effect of TAM, and the differences were statistically significant (TABLE 3). At the same time, there was an interaction effect between time and treatment programs.
| variable | F | p-value | |
|---|---|---|---|
| TAM | time | 236.72 | < 0.001** |
| time*treatment | 6.21 | 0.001** | |
| treatment | 6.61 | 0.014* |
**p<0.01; *p<0.05.
Table 3: Repeated Analysis of Variance of Tam
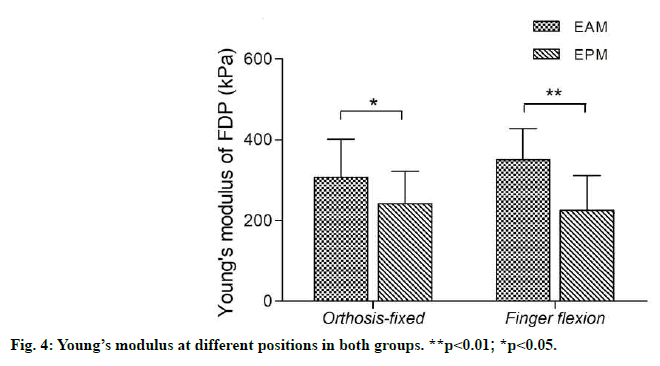
The orthosis-fixed position in the EPM group was at wrist flexion of 20° and the MP flexion of 60°, while that in the EAM group was a neutral wrist position and an MP flexion of 30°. In these two positions, there was a significant difference in Young’s modulus of the repaired FDP tendons. Young’s modulus of the FDP tendon was 351.42 kPa at partial active finger flexion status in the EAM group, which was significantly higher than that of passive finger flexion status in the EPM group (fig. 4).
Our study showed that patients in the EAM group had better functional recovery than those in the EPM group on total active motion (TAM) and functional grading by adjusted Strickland’s system. The TAM of the affected fingers after surgery was measured at multiple time points, and the repeated measurement method of the general linear model was used for analysis. The results showed that the treatment plan, time factor, and the interaction between these two elements had significant effects on functional recovery. The beneficial impact of digital function in the EAM group was observed, but not significant at four w after surgery, and the effect increased over time. These findings support the implementation of EAM as a post-operational rehabilitation protocol for patients with flexor tendon repaired in zone II.
However, researches conducted by Rigo[22] and Frueh[8] demonstrated an opposite result that active motion in the early phase post-surgery did not improve the overall long-term outcomes when compared with passive protocols. These controversy results could be interpreted as follows. In this present study, there was a small change in the immobilization position compared with the aforementioned researches, that the wrist and MP joints were placed in a slightly extended position in the EAM group. The increase of flexion angle of wrist and MP joints, which would reduce the tension of flexor tendon, might also reduce the efficiency of flexor tendon gliding distance. This postulation would explain why only simply add active motion in modified Kleinert protocol could not achieve better hand function.
Fundamental researches in recent y have shown that the healing of tendons incorporates two processes, an extrinsic healing process and an intrinsic one[23]. Extrinsic healing procedure promotes the invasion of fibroblasts and stimulates the formation of adhesion between the tendon and the surrounding tissues. By contrast, the intrinsic healing procedure promotes the formation of type I collagen, facilitates rearrangement and cross-linking of collagen inside the tendon, and increases the strength of tendons[24]. The application of proper tension on the repaired tendon promoted the intrinsic healing procedure and limited the extrinsic healing procedure, to enhance the integrity of the repaired tendon and prevent the formation of tendon adhesion[25]. Thus, active motion and immobilization in slightly extension position may contribute to beneficial functional recovery in post-operational patients with complete lacerations of flexor tendons in zone II via maintaining proper tension in the compromised tendons.
It was worthwhile mentioning that the therapist needed to be aware of the postoperative swelling and scar formation, and corresponding treatment should be emphasized in the whole procedure, such as edema control and scar massage. Primarily attention should be focused on swelling in the first two w, and exercise movement in both groups should be adjusted individually according to the degree of swelling.
Previous clinical studies on flexor tendon repair showed that the incidence of secondary rupture ranged from 0.9 % to 5 %, with active rehabilitation program higher than passive ones[26-29]. There was no secondary rupture observed in both groups in the present study, which demonstrated the safety of both treatment regimens. Based on our experience, we provided a few recommendations to ensure the safety of treatments. Firstly, patients’ understanding and compliance should be fully considered before treatment. For instance, patients in the EAM group should stop the partial finger active flexion immediately, when they encounter resistance, to prevent rupture of repaired flexor tendon caused by excessive tension. Therefore, patients need to have a sufficient understanding to perform partial finger active flexion for safety concerns of rehabilitation treatment. Secondly, we adopted the passive-flexion and active-extension sequential motion in the EAM group to reduce the viscous resistance via the warmup of passive activities, which increased the motion range of active digital flexion and decreased the risk of secondary ruptures.
The EAM group showed beneficial effects both in grip strength and grip strength ratio, indicating that EAM was crucial in protecting muscle function of extrinsic flexors in the forearms. However, there was no significant difference in pinching strength and pinching strength ratio between the groups. A plausible explanation may be that the primary dynamic muscles of pinching motion were the intrinsic muscles of the hand, and the injury of the digital flexor tendon may not directly affect the function of the intrinsic muscles. The DASH score of the EAM group was superior to that in the EPM group, but with no statistical significance[30].
Shear wave elastography, a non-invasive, real-time and quantitative method, provided a reference for changes of tensions in flexor tendons by measuring the stiffness of flexor tendons. In the EAM group, the stiffness of the tendon was the highest during the partial active finger flexion, which was 351 kPa. When the affected hand was immobilized with an orthosis, the increase of tension in the flexor tendon could be induced by the extension of the wrist and fingers. By contrast, the flexor tendon was relaxed entirely in the passive finger flexion position, and the value of Young’s modulus was at its lowest. These findings supported the feasibility of SWE in monitoring the tension of flexor tendons as it could discriminate different position and dynamics of the flexor tendons. Further studies focusing on the relationship between stiffness and tension of FDP, as well as the safety threshold of Young’s modulus was therefore warranted.
This study is an RCT research to examine the effect of the truly active exercise rehabilitation program. Results of our study proved that early partial active finger flexion after flexor tendon repair is safe and effective, and it is superior to early passive motion both in range of digital motion and grip strength. Therefore, EAM should be recommended in post-operational patients with complete laceration of Zone-II flexor tendon. Additionally, the application of shear wave elastography in detecting flexor tendon tension appears feasible, although further validation is still needed.
Author’s Contribution
Jun Wang, Haifeng Shi and Jianan Li contributed to study design, study supervision, and final approval of the manuscript; Wei Chen and Dong Yang contributed to treat patients and keep them in follow-up; Zhengfeng Liu and Lei Qian contributed to all assessments; Jun Wang, Zhengfang Liu, Hiafeng Shi contributed to data analysis interpretation, and drafting.
Acknowledgements
This work was supported by the Science and Technology Foundation of Wuxi (N20192012) and Wuxi Modern Industry Development Fund Project (WX18IIAN011).
Conflict of interest
The authors report no conflicts of interest.t.
References
- Tang JB. Recent evolutions in flexor tendon repairs and rehabilitation. J Hand Surg (European Volume) 2019;43:469-73.
- Strickland JW, Glogovac SV. Digital function following flexor tendon repair in zone II: a comparison of immobilization and controlled passive motion techniques. J Hand Surg 1980;5:537-43.
- Strickland JW, Schmidt CC. Repair of flexor digitorum profundus lacerations: the Indiana method. Opera Tech Orthop 1998;8:73-80.
- Zhao C, Amadio PC, Momose T, Couvreur P, Zobitz ME, An K. Effect of synergistic wrist motion on adhesion formation after repair of partial flexor digitorum profundus tendon lacerations in a canine model in vivo. J Bone Joint Surg 2002;84:78-84.
- Kannas S, Jeardeau TA, Bishop AT. Rehabilitation following zone II flexor tendon repairs. Tech Hand Upper Extrem Surg 2015;19:2-10.
- Higgins A, Lalonde DH. Flexor tendon repair postoperative rehabilitation: the Saint John protocol. PRS Global Open 2016;4:e1134.
- Tang JB. Indications, methods, postoperative motion and outcome evaluation of primary flexor tendon repairs in Zone 2. J Hand Surg (European Volume) 2007;32:118-29.
- Frueh FS, Kunz VS, Gravestock IJ, Held L, Haefeli M, Giovanoli P, et al. Primary flexor tendon repair in zones 1 and 2: early passive mobilization versus controlled active motion. J Hand Surg 2014;39:1344-50.
- Farzad M, Layeghi F, Asgari A, Ring DC, Karimlou M, Hosseini SA. A prospective randomized controlled trial of controlled passive mobilization vs. place and active hold exercises after zone 2 flexor tendon repair. Hand Surg 2014;19:53-9.
- Neiduski RL, Powell RK. Flexor tendon rehabilitation in the 21st century: A systematic review. J Hand Ther 2019;32:165-74.
- Cao W, Sun Y, Liu L, Wang Z, Wu JY, Qiu L, et al. A Multicenter Large Sample Shear Wave Ultrasound Elastographic Study of the Achilles Tendon in Chinese Adults. J Ultras Med 2019;38:1191-200.
- Fu S, Cui L, He X, Sun Y. Elastic characteristics of the normal Achilles tendon assessed by virtual touch imaging quantification shear wave elastography. J Ultras Med 2016;35:1881-7.
- Sahr M, Sturnick DR, Nwawka OK. Quantitative Ultrasound Assessment of the Achilles tendon Under Varied Loads. J Ultras Med 2018;37:2413-8.
- Haen TX, Roux A, Soubeyrand M, Laporte S. Shear waves elastography for assessment of human Achilles tendon's biomechanical properties: an experimental study. J Mech Behav Biomed Materi 2017;69:178-84.
- Rees L, Matthews A, Masouros SD, Bull AMJ, Haywood R. Comparison of 1-and 2-knot, 4-strand, double-modified Kessler tendon repairs in a porcine model. J Hand Surg 2009;34:705-9.
- Trumble TE, Vedder NB, Seiler JG, Hanel DP, Diao E, Pettrone S. Zone-II flexor tendon repair: a randomized prospective trial of active place-and-hold therapy compared with passive motion therapy. J Bone Joint Surg 2010;92:138-9.
- Wang J, Erlandsson G, Rui YJ, Li-Tsang C. Efficacy of static progressive splinting in the management of metacarpophalangeal joint stiffness: a pilot clinical trial. Hong Kong J Occup Ther 2014;24:45-50.
- Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am J Ind Med 1996;29:602-8.
- Davis AW. On the effects of moderate multivariate nonnormality on Roy's largest root test. J Am Stat Assoc 1982;77:896-900.
- Mauchly JW. Significance test for sphericity of a normal n-variate distribution. Annal Math Stat 1940;11:204-9.
- Abdi H. The greenhouse-geisser correction. Encycl Res Design 2010;1:544-8.
- Rigó IZ, Haugstvedt JR, Røkkum M. The effect of adding active flexion to modified Kleinert regime on outcomes for zone 1 to 3 flexor tendon repairs. A prospective randomized trial. J Hand Surg (European Volume) 2017;42:920-9.
- Hope M, Saxby TS. Tendon healing. Foot Ankle Clin 2007;12:553-67.
- Sharma P, Maffulli N. Biology of tendon injury: healing, modeling and remodeling. J Musculoskel Neuron Interact 1900;6:181-90.
- Myer C, Fowler JR. Flexor Tendon Repair: Healing, Biomechanics, and Suture Configurations. Orthop Clin N Am 2016;47:219.
- Higgins A, Lalonde DH, Bell M, McKee D, Lalonde JF. Avoiding Flexor Tendon Repair Rupture with Intraoperative Total Active Movement Examination. Plast Reconstr Surg 2010;126:941-5.
- Chesney A, Chauhan A, Kattan A, Farokhyar F, Thoma A. Systematic Review of Flexor Tendon Rehabilitation Protocols in Zone II of the Hand. Plast Reconstr Surg 2011;127:1583-92.
- Starr HM, Snoddy M, Hammond KE, Seiler JG. Flexor Tendon Repair Rehabilitation Protocols: A Systematic Review. J Hand Surg 2013;38:1712-7.
- Karjalainen T, Jokinen K, Sebastin SJ, Luokkala T, Kangasniemi OP, Reito A. Correlations Among Objectively Measured Impairment, Outcome Classification Systems, and Subjectively Perceived Disability After Flexor Tendon Repair. J Hand Surg 2019;44:361-5.
- Pulos N, Bozentka DJ. Management of Complications of Flexor Tendon Injuries. Hand Clin 2015;31:293-9.