- *Corresponding Author:
- Lin An Wang
Department of Hepatobiliary Surgery, Jiuquan City People’s Hospital of Gansu Province, Jiuquan, Gansu 735000, China
E-mail: enfuzan0772@yeah.net
| This article was originally published in a special issue, “Modern Applications in Biomedical Research and Pharmaceutical Sciences” |
| Indian J Pharm Sci 2022:84(3) Spl Issue “202-206” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
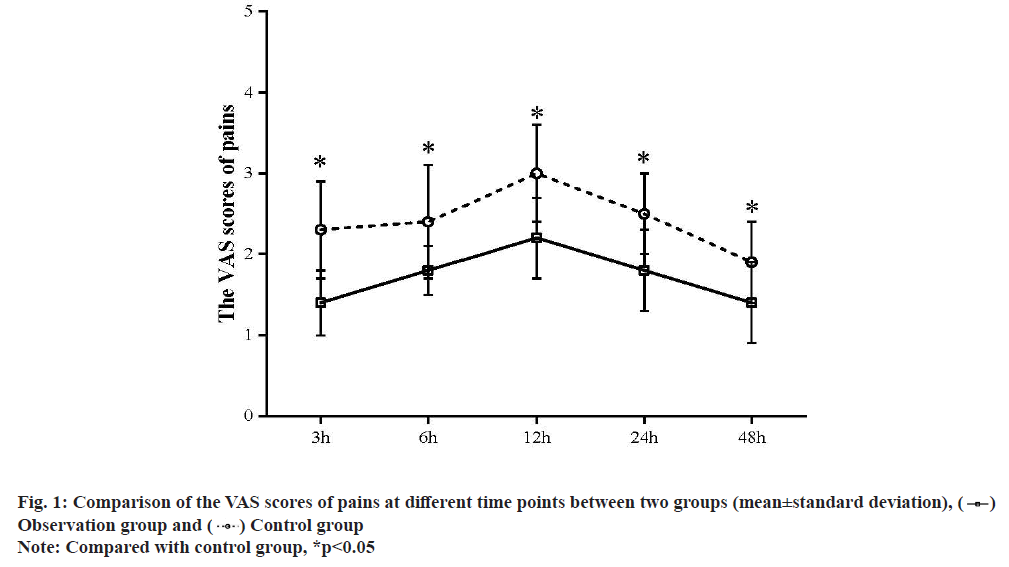
To analyze the analgesic effect of flurbiprofen axetil in combination with fentanyl on the patients after laparoscopic cholecystectomy is the objective of the study. Between April 2020 and April 2021, a total of 120 patients who received the delayed or scheduled laparoscopic cholecystectomy were enrolled into this study and divided into the control group and observation according to their admission sequence, with 60 patients in each group. Patients in the control group received the fentanyl for postoperative analgesia, while those in the observation group received the flurbiprofen axetil in combination with fentanyl. The visual analogue scale scores of patients in the observation group at postoperative 3 h, 6 h, 12 h, 24 h and 48 h were (1.4±0.4) points, (1.8±0.3) points, (2.2±0.5) points, (1.8±0.5) points and (1.4±0.5) points, significantly lower than (2.3±0.6) points, (2.4±0.7) points, (3.0±0.6) points, (2.5±0.5) points and (1.9±0.5) points in the control group (t=6.618, 4.244, 5.489, 5.218 and 3.728, p<0.05). Following operation, the ratio of patients requiring more analgesics in the observation group was only 5.0 %, far lower than 28.3 % in the control group (χ2=7.467, p<0.05). Besides, the difference in the incidence rates of the adverse reactions between two groups showed no statistical significance (p>0.05). As for the hemodynamic indexes (mean arterial pressure, oxygen saturation and heart rate), differences were only found in comparison of heart rate (p<0.05), instead of mean arterial pressure or oxygen saturation (p>0.05) at postoperative 3 h, 6 h, 12 h, 24 h and 48 h between two groups. For patients undergoing the laparoscopic cholecystectomy, combination of flurbiprofen axetil and fentanyl for postoperative analgesia can mitigate the pains within 2 d and reduce the additional demand for analgesics.
Keywords
Laparoscopic cholecystectomy, postoperative analgesia, flurbiprofen axetil, fentanyl
Laparoscopic cholecystectomy is preferred in the treatment of cholecystitis and gallstone with the excellent efficacy. Due to the variation in the age, structure of population and the increase in pathogenic factors, a rapid increase has also witnessed in the prevalence of gallbladder diseases, which also contribute to the acute increase in the population of patients undergoing the laparoscopic cholecystectomy[1]. Laparoscopic cholecystectomy, though exceling in mitigating the pains, still belongs to the traumatic surgery that inevitably results in the postoperative pains, stress response and complications, affecting the prognosis remarkably[2]. So, postoperative pain management, as the major part consisting of the quality management of laparoscopic cholecystectomy, usually take fentanyl for postoperative analgesia, but fentanyl, due to the extremely high incidence rate of adverse reactions, is limited in clinical practice. Flurbiprofen axetil is a common analgesic that is frequently used in the orthopedic surgery, but scarcely in combination with fentanyl. Some researchers believed that laparoscopic surgery results in mild pains, with no demand for the preemptive analgesia[3,4]. In this casecontrol study, we selected a total of 120 patients undergoing the scheduled or delayed laparoscopic cholecystectomy in this hospital to evaluate the value of flurbiprofen axetil in combination with fentanyl and the detailed information is reported as follow. Between April 2018 and April 2019, a total of 120 patients who received the delayed or scheduled laparoscopic cholecystectomy were selected according to the following criteria. Inclusion criteria include patients undergoing the scheduled surgery; patients in a low transfer risk; patients with no history of preoperative abdominal drainage and with the non-critical disease; patients agreeing to participate in the study after they were informed of the protocol. Exclusion criteria include patients undergoing the combined surgery; patients with the history of surgery in lower abdomen (not including caesarean section); patients with peritonitis; patients with contraindications including portal hypertension; patients with the suspicious contraindication of medication in gastrointestinal tract. 120 subjects were randomly divided into control group and observation group, with 60 cases in each group. There was no significant difference in age, sex, Body Mass Index (BMI) level and gallbladder atrophy between the two groups (p>0.05, Table 1). The study has been approved by the hospital ethics committee and the patients and their families have informed consent to the study. Before surgery, patients were trained to utilize the method for evaluating the pains by Visual Analogue Scale (VAS). At 1 h prior to surgery, patients were given with 100 mg pentobarbital sodium (Saudi Food and Drug Authority (SFDA) Approval No.: H31020532) and 0.5 mg atropine (SFDA Approval No.: H32020236), followed by the regular monitoring and endotracheal intubation. Patients were anesthetized by 0.05 mg/kg midazolam (SFDA approval No.: H20041106), propofol at dose to maintain the plasma concentration within 2.0 and 3.0 μg/ml and fentanyl (SFDA approval No.: H20143314) at dose of 2.0 μg/kg and vecuronium bromide (SFDA approval No.: H20063411) at dose of 0.12 mg/kg. 4 min later, endotracheal intubation was performed for the patients, followed by the mechanical ventilation. For patients in the control group, fentanyl at a dose of 2.0 μg/kg was given via intravenous injection at 45 min after skin preparation. Patients in the observation group received the flurbiprofen axetil (SFDA Approval No.: H20041508) at dose of 1 mg/kg respectively at 10 min prior to skin preparation and after surgery. We observed and recorded the VAS scores of pains, hemodynamic indicators, and ratio of demand for the additional analgesic drugs and the incidence of adverse reactions (nausea and vomiting) between two groups at 3, 6, 12, 24 and 48 h after surgery. Statistical Package for the Social Sciences (SPSS) 18.0 software and Web Processing Service (WPS) were utilized to process the data. VAS scores were in normal distribution, expressed in mean±standard deviation and compared between two groups or inside one group by use of the t test. Enumeration data were expressed by n (%) and compared by t test, p<0.05 suggested the statistical significance of difference. Comparison of the VAS scores of pains between two groups is shown below. In the observation group, the VAS scores at 3, 6, 12, 24 and 48 h after operation were all lower than those in the control group (p<0.05, fig. 1). Comparison of the ratio of demand for analgesics and incidence of adverse reactions between two groups was explained here. Following operation, the ratio of patients requiring more analgesics in the observation group was only 5.0 %, far lower than 28.3 % in the control group (χ2=7.467, p<0.05). Besides, the difference in the incidence rates of the adverse reactions between two groups showed no statistical significance (p>0.05, Table 2). Comparison of the hemodynamic indicators between two groups was shown below. As for the hemodynamic indexes (Mean Arterial Pressure (MAP), Oxygen Saturation (SpO2) and Heart Rate (HR)), differences were only found in comparison of HR (p<0.05), instead of MAP or SpO2 (p>0.05) at postoperative 3 h, 6 h, 12 h, 24 h and 48 h between two groups (fig. 2). Laparoscopic cholecystectomy often results in the stimulus pains in wound, pneumoperitoneum-related stimulus pains or tissue pains caused by the internal incision, with a VAS score ranging from 2 to 4 points, usually peaking at postoperative 12 to 24 h[5]. This was also confirmed in this study: Peak VAS scores in the observation group and the control group were attained at postoperative 12 h and from postoperative 24 h, VAS scores in two groups had acute decreases. According to the previous evidence and the results in the control group, regular analgesic method for laparoscopic cholecystectomy has the following features: The stimulus pain at wound associates mostly with the sensitization of the primary or secondary pains, which would be aggravated after the recovery from the anesthesia, while the regular analgesic measures, though preventing the severe pains, still could not manage the pains within the mild range (<3 points); pains after laparoscopic cholecystectomy are induced by various factors, persisting for a relative long time and patients at 48 h after surgery still complain about the residual pains, which, though being tolerated well, affects the life quality of patients[6,7]. As for the treatment of the pains after laparoscopic cholecystectomy, opioids are a common group of analgesics that usually result in the adverse reactions (nausea and vomiting), with an incidence rate between 4 % and 10 %[8]. In this study, the incidence rate of adverse reaction in the control group was 5.0 %, while the ratio of demand for analgesic was as high as 28.3 %, suggesting the insufficiency of fentanyl in pharmacokinetics that is associated with the dosedependent manner of fentanyl. Thus, controlling the dosage can maintain the VAS scores within 3 and 4 points, thus serving as the common method for clinical prophylaxis of adverse reactions. Currently, the analgesic effect of flurbiprofen axetil in combination with fentanyl has been widely acknowledged by the researchers. Some researchers analyzed the analgesic effect of this strategy in the laparoscopic resection for cholecystitis and found that it is able to reduce the dose of opioids, and the incidence rate of adverse reactions. In comparison with the single use of fentanyl, this strategy could further decrease the VAS score by 1 points and attain a peak score at 2 to 3 points. Similarly, we found that in the observation group, the peak VAS score was (2.2±0.5) points[9,10]. Importantly, differences remain in the appearance time of peak in VAS score of pain, ranging from preoperative 2 h to 48 h, mainly dependent on the pathogenesis of surgical pains. Thus, to cover the plateau of drug, we should take the pharmacokinetics and time of medication into consideration[11]. Flurbiprofen axetil is featured with the antipyretic and anti-inflammatory effects in addition to the analgesic effect, particularly appropriate for the treatment of inflammatory pains by accumulating selectively in the inflammatory tissues or vascular injury. For laparoscopic cholecystectomy, postoperative pains may be associated with the septic inflammation that can be managed effectively by flurbiprofen axetil to achieve the analgesic effect. Similarly, evidence from other literatures demonstrates that co-administration can reduce the dose of opioids but improve the analgesic effect. At present, flurbiprofen axetil also combines with the tramadol, sufentanil and dexmedetomidine that can improve the efficacy of flurbiprofen axetil to maintain the postoperative pains within the tolerable range (1 to 3 points)[12,13]. Furthermore, analgesic effect of flurbiprofen axetil also correlates with the usage and dosage. In this study, preemptive and postoperative analgesia, with a higher satisfaction rate, can theoretically reduce the intraoperative stress response of extubation and maintain the relatively stable hemodynamics[14]. For laparoscopic cholecystectomy, patients also suffer the pains caused by the absorbance of Carbon dioxide (CO2) in addition to the inflammation and single medication can hardly gain any ideal efficacy. Besides, flurbiprofen axetil can also suppress the synthesis of prostaglandin to exert the analgesic effect, which, however, would affect the bone union in youth. Thus, in addition to achieving the analgesic effect, physicians should additionally consider to reduce the dose of flurbiprofen axetil in analgesia for young patients. The results of this study showed that the VAS scores of patients in the observation group at postoperative 3 h, 6 h, 12 h, 24 h and 48 h were significantly lower than those in the control group (p<0.05). Following operation, the ratio of patients requiring more analgesics in the observation group was only 5.0 %, far lower than 28.3 % in the control group (χ2=7.467, p<0.05). Besides, the difference in the incidence rates of the adverse reactions between two groups showed no statistical significance (p>0.05). As for the hemodynamic indexes (MAP, SpO2 and HR), differences were only found in comparison of HR (p<0.05), instead of MAP or SpO2 (p>0.05) at postoperative 3 h, 6 h, 12 h, 24 h and 48 h between two groups. For patients undergoing the laparoscopic cholecystectomy, combination of flurbiprofen axetil and fentanyl for postoperative analgesia can mitigate the pains within 2 d and reduce the additional demand for analgesics.
| Group | Sex (male/female) | Age (y) | BMI level (kg/m2) | Gallbladder atrophy (number) |
|---|---|---|---|---|
| Observation group | 26/34 | 51.3±11.4 | 22.5±2.2 | 6 |
| Control group | 27/33 | 50.5±12.7 | 22.2±2.5 | 8 |
Table 1: Comparison of General Data between The Two Groups (x±s)
| Group | N | Demand for analgesics | Nausea and vomiting | Somnolence | Respiratory inhibition | Total |
|---|---|---|---|---|---|---|
| Observation group | 60 | 3 (5.0) | 2 (3.3) | 2 (3.3) | 1 (1.7) | 5 (8.3) |
| Control group | 60 | 17 (28.3) | 2 (3.3) | 1 (1.7) | 0 | 3 (5.0) |
| χ2 | 7.442 | 0.513 | 0.276 | 0 | 0.218 | |
| p | 0.06 | 0.474 | 0.237 | 1 | 0.639 |
Table 2: Comparison of The Ratio of Demand for Analgesics and Incidence of Adverse Reactions between Two Groups [n (%)]
Author’s contributions:
Xiufeng Chu and Lu Liang contributed equally to this work.
Conflict of interests:
The authors declared no conflict of interest.
References
- Xing GQ, Yin DL, Yang HY, Song X, Liu LX. Advances in the diagnosis and treatment of acute non-calculous cholecystitis in the elderly. Chin J Pract Surg 2015;35(9):1011-3.
- Tang S, Wang H, Jiang JJ, Lin MB, Yin L. Effects of different treatment strategies on clinical outcomes of moderate to severe acute cholecystitis. Int J Dig Dis 2015;35(6):425-7.
- Chinese Pharmacopoeia Commission. Clinical application guidelines of drugs guidelines. Beijing: People’s Medical Publishing House; 2005. p. 101-4.
- Fritz HG, Holzmayr M, Walter B, Moeritz KU, Lupp A, Bauer R. The effect of mild hypothermia on plasma fentanyl concentration and biotransformation in juvenile pigs. Anesth Analg 2005;100(4):996-1002.
[Crossref] [Google Scholar] [PubMed]
- Wang HT. Comparison of analgesic effects of dexmedetomidine and flurbiprofen axetil combined with sufentanil in elderly patients with spinal surgery. China Matern Child Health Study 2017;28 (1):309-10.
- Topacoglu H, Karcioglu O, Cimrin AH, Arnold J. Respiratory arrest after low-dose fentanyl. Ann Saudi Med 2005;25(6):508-10.
- Zheng TT, Bai L, Yi Y, Xing Y, Tu F, Zhen JC. Study on the effect of different doses of flurbiprofen axetil combined with sufentanil on postoperative patient-controlled intravenous analgesia. Chin J Hosp Pharm 2018;38(8):850-3.
- Haj-Mirzaian A, Kordjazy N, Amiri S, Haj-Mirzaian A, Amini-Khoei H, Ostadhadi S, et al. Involvement of nitric oxide-cyclic guanosine monophosphate pathway in the antidepressant-like effect of tropisetron and ondansetron in mice forced swimming test and tail suspension test. Eur J Pharmacol 2016;780:71-81.
[Crossref] [Google Scholar] [PubMed]
- Zhou Z, Zhang MF, Yuan JY, Yuan WY, Xu LZ, Lei WJ. J Nurs 2017;24(19):47-51.
- Khalifeh S, Fakhfouri G, Mehr SE, Mousavizadeh K, Dehpour AR, Khodagholi F, et al. Beyond the 5-HT3 receptors: A role for α7nACh receptors in neuroprotective aspects of tropisetron. Hum Exp Toxicol 2015;34(9):922-31.
[Crossref] [Google Scholar] [PubMed]
- Yang K. Clinical analysis of flurbiprofen axetil injection combined with sufentanil intravenous infusion for postoperative analgesia. Chin Med Sci 2017;7(14):93-5.
- Yokoyama T, Yamashita K, Manabe M, Sluka KA. Tracheobronchomalacia-like lung collapse during three separate trials of general anesthesia. Anesth Analg 2006;103(4):1039-40.
[Crossref] [Google Scholar] [PubMed]
- Yu X, Fan ZL. Flurbiprofen ester sufentanil combined with different doses of dexmedetomidine for postoperative analgesia of laparoscopic gastric cancer. Chin Med Clin J 2017;17(7):1007-10.
- Ying L, Li SY, Lin PC. Effect of induction of dizosin combined with flurbiprofen axetil on recovery period of general anesthesia for lower abdominal surgery. Chin Foreign Med Res 2017;15(11):52-3.
 ) Observation group and (
) Observation group and ( ) Control group
) Control group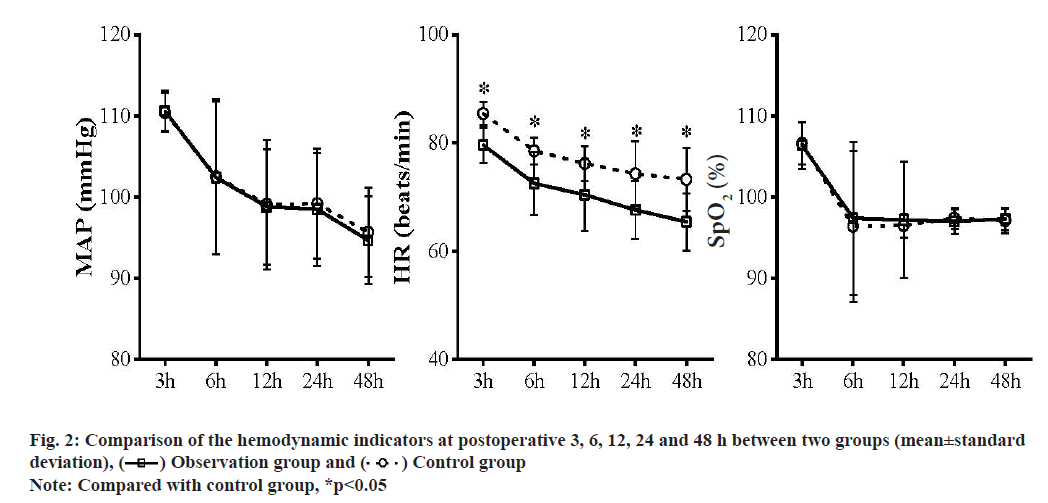
 ) Observation group and (
) Observation group and ( ) Control group
) Control group



