- *Corresponding Author:
- Shriya Ginde
Department of Oral and Maxillofacial Surgery, Vidyapeeth, Pune, Maharashtra 411018,
India
E-mail: drshriyagindesable@gmail.com
| Date of Received | 22 June 2022 |
| Date of Revision | 24 August 2023 |
| Date of Acceptance | 25 March 2024 |
| Indian J Pharm Sci 2024;86(2):517-524 |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
The most common oral and maxillofacial procedure is surgical removal of impacted third molars, which often results in post-operative inflammatory changes. Many pharmacological and nonpharmacological measures have been tried, to help resolve the same with minimum side effects to patients. Non pharmacological measures are surgery, cryotherapy amongst many others. Pharmacological measures include enzymatic or non-enzymatic preparations like antibiotics, steroids and various analgesic drugs. One such newer preparation is that of bromelain, which is an extract from the pineapple stem and plant. It is rich in thiol endopeptidases, cellulose, glycoproteins and carbohydrates. Bromelain has been very commonly used in a lot of medical interventions like sinusitis, thrombophlebitis, surgical trauma, pyelonephritis, angina pectoris, bronchitis as well as for enhancing absorption. It’s direct effect on bradykinin receptors has been affiliated to its analgesic property though it can also be due to its anti-inflammatory action. Research has shown that swelling, time required for healing, pain, bruising is reduced due to its property to digest fibrin; enabling reduced oedema post-operatively. Various dosages of the drug have been used to verify its efficacy but there is no consensus on exact optimum dosages. Hence in this study we aim at determining optimum dosage for bromelain providing an ideal maximum effect to reduce inflammation after removal of impacted third molars.
Keywords
Bromelain, inflammation, third molar, surgery
Oral and maxillofacial surgery is a branch where myriad of procedures are performed, however removal of third molars surgically is the most common out-patient procedure, involving an inflammatory sequelae due to the handling of hard and soft tissues[1]. Inflammation after surgery results in discomfort due to pain, reduced mouth opening and swelling[2]. These symptoms are based on factors like difficulty index of tooth extracted, technique utilised[2], handling of tissues, duration of surgery, incision used[3] and others. Factors like age, gender, body mass index could also be contributing to the after effects[4]. Studies by Osunde et al.[5] suggested that post surgery outcomes may however be independent of these factors. Inflammation occurring after surgeries is due to thromboxane related products, leukotrienes and prostaglandins as a result of conversion of phospholipids into arachidonic acid by Phospholipase A2 (PLA2)[2]. Minimizing this assures successful surgical practice. English medical literature has mentioned various methods being implemented to control the post-surgery swelling in patients undergoing surgeries for third molars including kinesiotapes and drains of various types[6] to varied pharmacological measures to reduce inflammatory response[7]. These range from enzymatic preparations to steroids, antibiotics, modified surgical procedures and cryotherapy to name a few[3]. Pharmacological measures like antibiotics are used to treat and prophylactically control infections that may be distant from surgical site or for controlling postoperative discomfort[3]. Pre-surgery antibiotic mouthwashes have been advised by Cho et al[8]. Corticosteroids are effective agents to control fluid transudation, swelling and inflammation after surgeries, however hazardous effects preclude their use[3]. These include betamethasone (anecdotal use), methylprednisolone acetate and sodium succinate (Intravenous (IV)/ Intramuscular (IM)), dexamethasone (orally), dexamethasone acetate (IM) and sodium phosphate (IV/IM)[3]. Many enzymatic preparations have been used for reducing postoperative inflammation. One such newer enzyme preparation is bromelain, a pineapple product. Pineapple (Ananas comosus) is a crucial member of the Bromeliceae family, and its extracts, especially bromelain, have been commonly used as a phytomedical agent since as early as 1875. It is a concoction of thiol endopeptidases, cellulose, glycoproteins and carbohydrates obtained from the plant stem and fruit. It has been used for treating sinusitis, thrombophlebitis, surgical trauma, pyelonephritis, angina pectoris, bronchitis and for enhancing antibiotic absorptions[9].
Bromelain’s direct effect on bradykinin receptors has been associated to its analgesic property though it can also be attributed to its anti-inflammatory action[7]. Research has shown that swelling, time required for healing, pain and bruising is reduced due to its property to digest fibrin enabling in reducing oedema after the surgery. However, it prevents fibrin formation in the coagulation pathway[7]. Many studies including a systematic review by Almeida et al.[10] suggest that bromelain can be effectively used for controlling inflammatory response after impacted third molar removal surgeries. However there is no consensus in English literature regarding dosages of bromelain used[10]. Studies have shown that body can absorb up to 12 g/d of bromelain devoid of any side effects[9]. Hence this study was conducted to determine optimum dosage of bromelain providing an ideal maximum anti-inflammatory effect after third molar surgeries.
Materials and Methods
This prospective, preliminary, double blinded study was carried out in oral and Maxillofacial surgery department. All 30 patients (18-40) y of age, requiring extraction of mandibular third molars, under local anaesthesia, with a Pederson’s difficulty index of 5-6 (moderately difficult cases); were included in this study. These patients were randomly divided into 3 groups of 10 patients each who were prescribed rescue analgesic as tablet paracetamol 500 mg PARACIP-500, lower parel, Mumbai and were compared with other two other groups who were prescribed capsule 500 mg of bromelain Health vit High Potency, West-Coast Pharmaceutical Works Ltd., Gota, Ahmedabad, Gujarat. Subjects in group 1 and 2 received 500 mg bromelain capsule 12 per h and 6 h respectively. Group 3 was prescribed tablet Paracetamol 500 mg as a rescue drug. All patients chosen for the study who were willing to participate were systemically healthy, without any systemic disorders (uncontrolled diabetes or hypertension, radiotherapy or bleeding disorders) and were not on any drug therapy that would interfere with inflammatory response (steroid therapy, antimicrobial or cancer chemotherapy). Only those willing for follow-up were included. A random allocation of patients was done using the opaque sealed envelope method, with patients and operating surgeon unaware of the drug composition prescribed. The study was conducted between July 2019 to August 2020 at the department of oral and maxillofacial surgery and was begun after Institutional Ethics Committee on Human Research Approval (Ref. No. DYPDCH/ IEC/123/132/19). Study abided by the Helsinki Declaration and its amendments; by the ethical guidelines by the institution.
Surgical procedure:
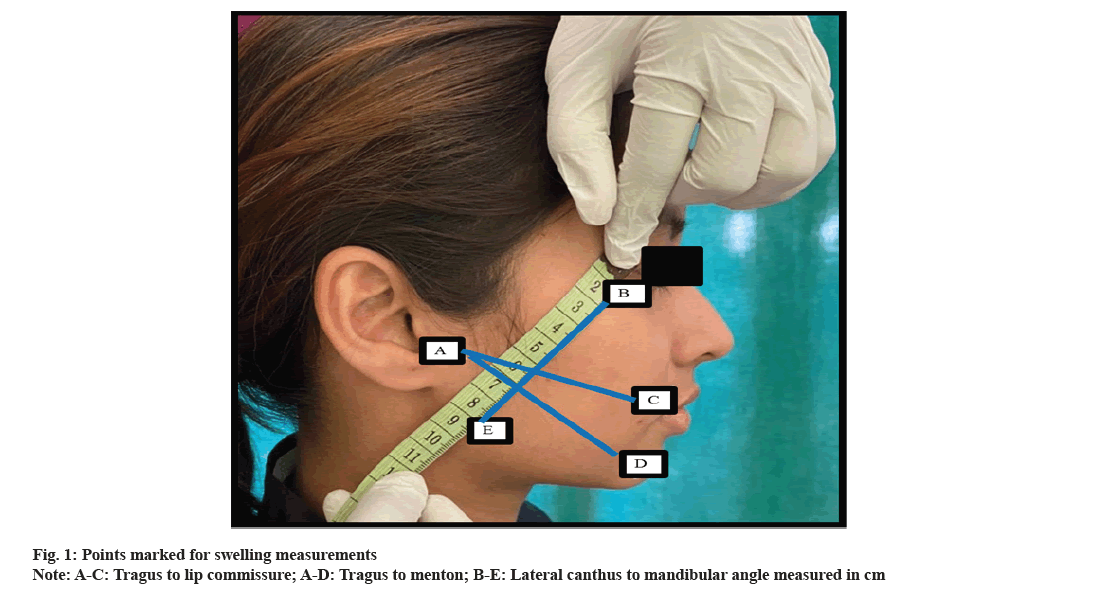
Those patients fitting into the inclusion criteria were taken a detailed history and valid written informed consent, pre-operative photos and radiographs were obtained. Assessment of the difficulty indices of impacted third molars was done. Surgical removal of the impacted third molars was done using standard surgical procedures. Sutures were removed on 7th follow-up day. Pain with the aid of Visual Analogue measurement Scale (VAS) was evaluated immediately post-surgery and facial swelling was measured on post-surgery 24 h and 7th day interval. Facial swelling was measured with 3 point measurement scale using a measurement tape (AC–tragus to lip commissure, AD–tragus to menton, BE–lateral canthus to mandibular angle), measured in cm [11](fig. 1).
Statistical analysis:
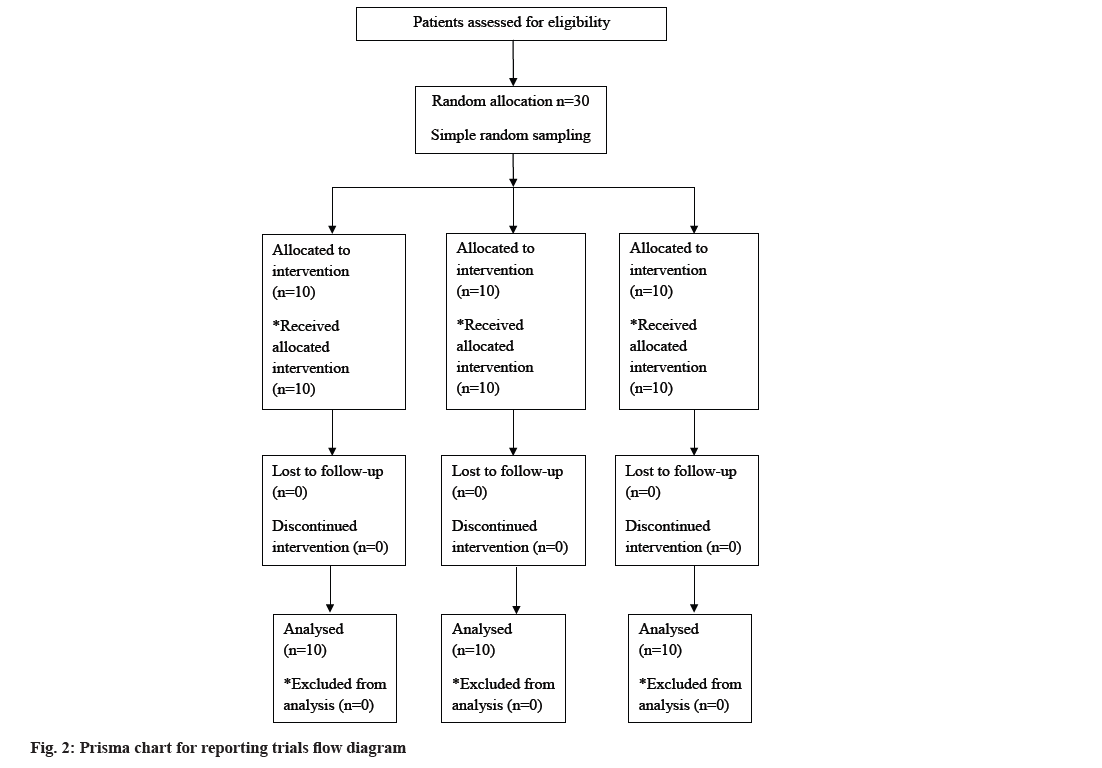
Allocation of the drugs was done using opaque sealed envelopes and patients were divided into ascertained groups by simple random sampling technique (fig. 2). Data was collected, compiled and entered in Microsoft Excel sheet and was analyzed using International Business Machines (IBM) Statistical Package for the Social Sciences (SPSS) version 21, Chicago, United States of America. For comparison within groups, repeated measures Analysis of Variance (ANOVA) followed by post hoc test was applied. Between groups one way ANOVA followed by post hoc test was applied. A value of p<0.05 was considered to be significant statistically.
Results and Discussion
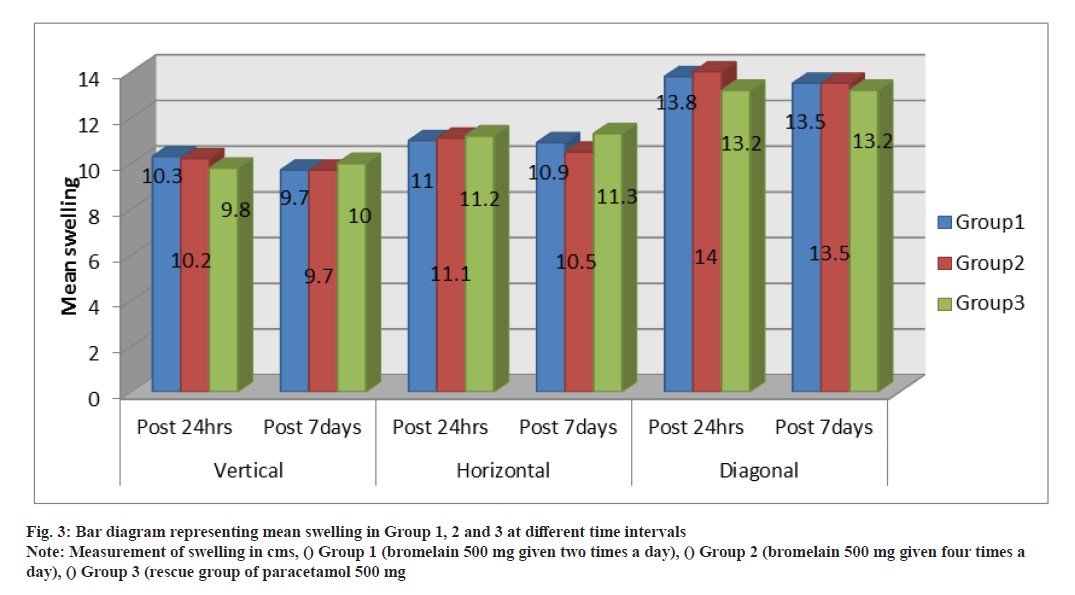
In this experimental study, patients were randomly allocated to their groups and were prescribed bromelain capsule and analgesics were examined after the surgery for pain and swelling on the 1st and 7th d intervals. Group 1 and 2 were prescribed bromelain capsules 500 mg at 12 h and 6 h a day respectively, after the surgery. Group 3 received rescue analgesics. All the above mentioned drugs were advised for a 7 d period. Patients were examined for swelling and pain on 24 h and 7 d post-surgery intervals. Paired t-test was used to assess the differences in swelling measurements from 24 h and 7th d interval postsurgery and it revealed considerable difference (value of p<0.05) for vertical (0.003) and diagonal (0.024) values in group 1, vertical (0.004) and horizontal (0.006) values in group 2. No noteworthy differences were observed in the vertical, horizontal or diagonal dimensions in group 3 (Table 1 and fig.3).
| Groups | Swelling measurement | Mean difference | Significance (p) |
|---|---|---|---|
| Group 1 | Vertical | 0.550* | 0.003* |
| Horizontal | 0.1 | 0.16 | |
| Diagonal | 0.3 | 0.024* | |
| Group 2 | Vertical | 0.450* | 0.004* |
| Horizontal | 0.570* | 0.006* | |
| Diagonal | 0.45 | 0.159 | |
| Group 3 | Vertical | 0.2 | 0.168 |
| Horizontal | 0.15 | 0.193 | |
| Diagonal | 0.00 | 1.00 |
Note: *Significance at p<0.05 and t: test to assess the difference within groups at time intervals
Table 1: Difference of swelling within the groups at time intervals between 24 h and 7th post-operative d
One way ANOVA revealed no notable distinction at 24 h and 7th d post-operative interval between the groups for vertical, horizontal and diagonal dimensions of swelling (Table 2). Assessment of pain was done using repeated measures ANOVA which demonstrated considerable differences within each group between various time frames. Immediate pain intensity in group 1 was 6.6±1.2, group 2 was 6.3±2.1 and group 3 was 7.6±1.6, with p value of 0.207. For the post-surgery 24 h interval in group 1, 2 and 3 it was 6.2±1.2, 5.3±1.8 and 6.1±0.9 respectively with a p value of 0.276. For the 7th d post-surgery in the 3 groups it was 1.2±1.0, 0.8±0.6 and 3.3±1.4 respectively with p value of <0.0001. No significant differences were found between the groups using one way ANOVA at different time intervals. However a remarkable difference (<0.0001) was present between the groups on 7th post-surgery follow-up day (Table 3).
| Time interval | Measurement | F value | Significance |
|---|---|---|---|
| Post-operative 24 h | Vertical | 0.559 | 0.578 |
| Horizontal | 0.057 | 0.945 | |
| Diagonal | 1.325 | 0.282 | |
| Post-operative 7 d | Vertical | 0.172 | 0.843 |
| Horizontal | 1.688 | 0.204 | |
| Diagonal | 0.18 | 0.837 |
Note: No significant difference was observed between the groups at vertical, horizontal and diagonal swelling size at post-operative 24 h as well as post-operative 7 d
Table 2: Difference between the groups for swelling at 24 h and 7 d
| Time interval | Group1 | Group 2 | Group 3 | F value | Significance(p) |
|---|---|---|---|---|---|
| Immediate | 6.6±1.2 | 6.3±2.1 | 7.6±1.6 | 1.67 | 0.207 |
| Post-operative 24 h | 6.2±1.2 | 5.3±1.8 | 6.1±0.9 | 1.352 | 0.276 |
| Post-operative 7 d | 1.2±1.0 | 0.6 | 3.3±1.4 | 15.56 | <0.0001* |
| F value | 40.52 | 24.03 | 14.39 | - | - |
| Significance (p) | <0.0001* | <0.0001* | <0.0001* | - | - |
Note: *Significance at p<0.05 and significant difference was found within Group 1, Group 2 and Group 3 with respect to time intervals. Significant difference was found between the groups at post-operative 7 d. Repeated measure ANOVA within the group one way ANOVA between the groups
Table 3: Pain intensity in group 1, 2 and 3 at different time intervals
Application of post-hoc Bonferroni test revealed considerable difference between immediate to postsurgery 7th d time frame and post-surgery 24 h to post-surgery 7th d interval in all the aforementioned groups. A significant difference in pain score was found only at 7th d post-surgery interval between the groups. Tukey-Honestly Significant Difference (HSD) revealed significant differences between group 1-group 3 with a mean difference of 2.100 and <0.0001 and group 2-group 3 with mean difference of 2.50 and p value of <0.0001(Table 4).
| Groups | Time | Mean Difference | Significance (p) |
|---|---|---|---|
| Group 1 | Immediate-post Op 7 days | 5.400 | <.0001* |
| Post Op 24hrs- Post Op 7 days | 5.000 | <.0001* | |
| Group2 | Immediate- Post Op 7days | 5.500 | <.0001* |
| Post Op 24hrs- Post Op 7 days | 4.500 | <.0001* | |
| Group3 | Immediate- Post Op 7days | 4.300 | .001* |
| Post Op 24hrs- Post Op 7 days | 2.800 | .002* | |
| Immediate -Post Op 24hrs | 1.500 | .046* |
Note: *Significance at p<0.05 bonferroni for post hoc within the group; significant difference in pain score was found only at 7th post-operative d between the groups. Tukey HSD revealed a significant difference between Group1-Group3 with mean difference of 2.100 and <0.0001 and Group2-Group3 with mean difference of 2.50 and p<0.0001.
Table 4: Differences of pain intensity within group 1, 2 and 3 at different time intervals
Thus it can be noted that pain intensity was maximum in group 3, followed by group 1 and then group 2. It shows that groups with capsule bromelain prescribed 6 h had superior pain reduction compared to the other two groups. As for swelling, all groups showed comparable reduction in the follow-up examination.
A similar study was conducted by Gupta et al.[12] where they compared aceclofenac and bromelain prescribed to patients after surgical removal of impacted lower third molar and they summarised that bromelain has effective action to control inflammation and that it also has comparative pain relieving effects when compared to aceclofenac along with reduced unsolicited consequences[12]. Another study promulgated a decrease in inflammation and an improvement in the opening of mouth in patients that received bromelain as against the ones who were in control group of the same dosage as of the drug. They summarised that even with lower dosages administered over a longer duration of time, anticipated effects could be achieved. They affirmed that bromelain may be useful in decreasing associated inflammation, may help in improving mouth opening when prescribed in proper dosages after surgeries of third molars[13].
Researchers also compared 4 groups in which first group received no drug, second group had bromelain 40 mg at 6 h intervals for 6 d, third group was administered submucosal dexamethasone sodium phosphate pre-operatively and a fourth group with a combination of both the drugs of group 1 and 2, prescribed for 6 d. They proposed that third and fourth group showed notable decrease in swelling of the face, whereas in the second group swelling reduction was present when aided with rescue painkiller consumption. Limited positive effects were noted on mouth opening when compared with control group. They concluded that though the drug has a limited effect on mouth opening, when combined with a steroid, results were superior and a combination of the these two drugs could thus work wonders in reducing inflammation after surgery[2].
In a systematic review conducted by Almeida et al.[10] they summed up that bromelain compared to other analgesic groups did not show any superior results for post-surgery swelling or mouth opening, however better results were attained with regards to pain control and reduction in morbidity. Nascimento- Júnior et al.[14] supported their review whereby they suggested that bromelain had minimal effect on the reduction of swelling and that there was lack of data on the safety of use of this drug. They however affirmed that the drug helped in improving patient’s daily life. Pavan et al.[9] in their reviews promulgated that the drug could be safely consumed upto 12 g/d, devoid of any effects.
Another systematic review suggested that bromelain with its minimal effects after consumption could be used as an alternative to steroids or painkillers[15], which was backed with the studies conducted by de Souza et al.[16]. Bromelain also could be used effectively alongside antibiotics like amoxicillin to control pain and facial swelling after surgeries[17]. Similar supportive data was produced by Moffa et al.[18], however they suggested more such studies be conducted for affirmation of the same. Multitude of studies have been conducted on various allopathic drugs like aceclofenac and diclofenac being advised after surgeries of third molars and how one drug is better than the other[19]. Similar comparisons had been done between ketoprofen and bromelain[20] or diclofenac sodium and bromelain[21] where the latter was found to be similar in effects to these age-old painkillers being used. Lately various plant based products are also being used after these surgeries and have warranted good results compared to traditional medications[22]. Combinations of these herbal products including bromelain and traditional drugs have also been done by various authors and have found bromelain singly to have comparable results in controlling after effects of the surgery[1]. This drug has been very commonly used in various other fields to reduce swelling after surgeries, osteoarthritis, bowel diseases with inflammatory changes[23], burns dressings, topical use[24] and so on. Studies have also shown how bromelain can be used successfully for patients with a known history of tumors of haematologic origin, patients with ongoing chemotherapy, who have to undergo surgery for third molars[25] or orthognathic like major oral surgeries[26]. Studies by Bormann et al. have suggested that higher dosages of the drug may not be having any different effects when compared to lower drug dosages [27].
However there is paucity of data on the optimum dosages required for the maximum beneficial outcome from the drug. Hence our study was conducted to evaluate the optimum dosage of bromelain that would effectively reduce inflammatory effects in the form of pain and swelling after third molar surgeries. Results from our study indicate that pain reduction was maximum with bromelain capsule 500 mg prescribed 6 h as compared to the other two groups. As for the decrease in swelling, results were comparable in all the three groups. Thus dosages of 500 mg 12 h or 6 h both can be effectively be used as a comparable alternative to the age-old analgesics, for patients undergoing surgeries for third molars. However more such studies to confirm dosages of the drug will affirm their widespread use over traditional drugs and warrant better after surgery effects for the patients.
Conflict of interest:
The authors declare that there is no conflict of interest.
References
- Ordesi P, Pisoni L, Nannei P, Macchi M, Borloni R, Siervo S. Therapeutic efficacy of bromelain in impacted third molar surgery: A randomized controlled clinical study. Quintessence Int 2014;45(8).
[Crossref] [Google Scholar] [PubMed]
- Ghensi P, Cucchi A, Creminelli L, Tomasi C, Zavan B, Maiorana C. Effect of oral administration of bromelain on postoperative discomfort after third molar surgery. J Craniofac Surg 2017;28(2):e191-7.
[Crossref] [Google Scholar] [PubMed]
- Sortino F, Cicciù M. Strategies used to inhibit postoperative swelling following removal of impacted lower third molar. Dent Res J 2011;8(4):162.
[Crossref] [Google Scholar] [PubMed]
- de Santana-Santos T, de Souza-Santos JA, Martins-Filho PR, da Silva LC, e Silva ED, Gomes AC. Prediction of postoperative facial swelling, pain and trismus following third molar surgery based on preoperative variables. Med Oral Patol Oral Cir Bucal 2013;18(1):e65.
[Crossref] [Google Scholar] [PubMed]
- Osunde OD, Saheeb BD. Effect of age, sex and level of surgical difficulty on inflammatory complications after third molar surgery. J Maxillofac Oral Surg 2015;14:7-12.
[Crossref] [Google Scholar] [PubMed]
- Genc A, Cakarer S, Yalcin BK, Kilic BB, Isler SC, Keskin C. A comparative study of surgical drain placement and the use of kinesiologic tape to reduce postoperative morbidity after third molar surgery. Clin Oral Investig 2019;23:345-50.
[Crossref] [Google Scholar] [PubMed]
- de la Barrera-Núñez MC, Yáñez-Vico RM, Batista-Cruzado A, Heurtebise-Saavedra JM, Castillo-de Oyagüe R, Torres-Lagares D. Prospective double-blind clinical trial evaluating the effectiveness of Bromelain in the third molar extraction postoperative period. Med Oral Patol Oral Cir Bucal 2014;19(2):e157.
[Crossref] [Google Scholar] [PubMed]
- Cho H, Lynham AJ, Hsu E. Postoperative interventions to reduce inflammatory complications after third molar surgery: Review of the current evidence. Aust Dent J 2017;62(4):412-9.
[Crossref] [Google Scholar] [PubMed]
- Pavan R, Jain S, Kumar A. Properties and therapeutic application of bromelain: A review. Biotechnol Res Int 2012;2012.
[Crossref] [Google Scholar] [PubMed]
- de Ac Almeida R, de Sousa Lima FC, Vasconcelos BD. Is bromelain an effective drug for the control of pain and inflammation associated with impacted third molar surgery? Systematic review and meta-analysis. Int J Oral Maxillofac Surg 2019;48(5):651-8.
[Crossref] [Google Scholar] [PubMed]
- Abu-Mostafa NA. The effects of primary and secondary wound closure following surgical extraction of lower third molars on post-operative morbidity: A prospective randomized clinical trial. J Dent Oral Hygiene 2015;7(10):168-74.
- Gupta AA, Kambala R, Bhola N, Jadhav A. Comparative efficacy of bromelain and aceclofenac in limiting post-operative inflammatory sequelae in surgical removal of lower impacted third molar: A randomized controlled, triple blind clinical trial. J Dent Anesth Pain Med 2022;22(1):29.
- de la Barrera-Núñez MC, Yáñez-Vico RM, Batista-Cruzado A, Heurtebise-Saavedra JM, Castillo-de Oyagüe R, Torres-Lagares D. Prospective double-blind clinical trial evaluating the effectiveness of Bromelain in the third molar extraction postoperative period. Med Oral Patol Oral Cir Bucal 2014;19(2):e157.
[Crossref] [Google Scholar] [PubMed]
- do Nascimento-Júnior EM, Reinheimer DM. Efficacy of proteolytic enzyme bromelain on health outcomes after third molar surgery. Systematic review and meta-analysis of randomized clinical trials. Med Oral Patol Oral Cir Bucal 2019;24(1):e61.
[Crossref] [Google Scholar] [PubMed]
- Liu S, Zhao H, Wang Y, Zhao H, Ma C. Oral bromelain for the control of facial swelling, trismus, and pain after mandibular third molar surgery: A systematic review and meta-analysis. J Oral Maxillofac Surg 2019;77(8):1566-74.
[Crossref] [Google Scholar] [PubMed]
- de Souza GM, Fernandes IA, Dos Santos CR, Falci SG. Is bromelain effective in controlling the inflammatory parameters of pain, edema, and trismus after lower third molar surgery? A systematic review and meta-analysis. Phytother Res 2019;33(3):473-81.
[Crossref] [Google Scholar] [PubMed]
- Singh T, More V, Fatima U, Karpe T, Aleem MA, Prameela J. Effect of proteolytic enzyme bromelain on pain and swelling after removal of third molars. J Int Soc Prev Community Dent 2016;6(Suppl 3):S197.
- Moffa A, Fraccaroli F, Carbone S, Rinaldi V, Costantino A, Lopez MA, et al. Bromelain after oral or dental procedures: An update. J Biol Regul Homeost Agents 2019;33(5):1629-34.
[Google Scholar] [PubMed]
- Chunduri NS, Kollu T, Goteki VR, Mallela KK, Madasu K. Efficacy of aceclofenac and diclofenac sodium for relief of postoperative pain after third molar surgery: A randomised open label comparative study. J Pharmacol Pharmacother 2013;4(2):144-5.
[Crossref] [Google Scholar] [PubMed]
- Inchingolo F, Tatullo M, Marrelli M, Inchingolo AM, Picciariello V, Inchingolo AD, et al. Clinical trial with bromelain in third molar exodontia. Eur Rev Med Pharmacol Sci 2010;14(9):771-4.
[Google Scholar] [PubMed]
- Majid OW, Al-Mashhadani BA. Perioperative bromelain reduces pain and swelling and improves quality of life measures after mandibular third molar surgery: A randomized, double-blind, placebo-controlled clinical trial. J Oral Maxillofac Surg 2014;72(6):1043-8.
[Crossref] [Google Scholar] [PubMed]
- Isola G, Matarese M, Ramaglia L, Iorio-Siciliano V, Cordasco G, Matarese G. Efficacy of a drug composed of herbal extracts on postoperative discomfort after surgical removal of impacted mandibular third molar: A randomized, triple-blind, controlled clinical trial. Clin Oral Investig 2019;23:2443-53.
[Crossref] [Google Scholar] [PubMed]
- Bottega R, Persico I, De Seta F, Romano F, Di Lorenzo G. Anti-inflammatory properties of a proprietary bromelain extract (Bromeyal™) after in vitro simulated gastrointestinal digestion. Int J Immunopathol Pharmacol 2021;35:20587384211034686.
[Crossref] [Google Scholar] [PubMed]
- Abdul Muhammad Z, Ahmad T. Therapeutic uses of pineapple-extracted bromelain in surgical care-A review. JPMA: J P Med Assoc 2017;67(1):121.
[Google Scholar] [PubMed]
- Tan Y, Li P. Bromelain has significant clinical benefits after extraction of the third molar during chemotherapy in patients with hematologic tumor. Oncol Lett 2018;15(3):2962-6.
[Crossref] [Google Scholar] [PubMed]
- Shetty V, Mohan A. A prospective, randomized, double-blind, placebo-controlled clinical trial comparing the efficacy of systemic enzyme therapy for edema control in orthognathic surgery using ultrasound scan to measure facial swelling. J Oral Maxillofac Surg 2013;71(7):1261-7.
[Crossref] [Google Scholar] [PubMed]
- Bormann KH, Weber K, Kloppenburg H, Koch A, Meiser P, Gellrich NC. Perioperative bromelain therapy after wisdom teeth extraction–A randomized, placebo-controlled, double-blinded, three-armed, cross-over dose-finding study. Phytother Res. 2016;30(12):2012-9.