- *Corresponding Author:
- Y. Zhao
The Second Hospital of Jilin University, Changchun 130041, China
E-mail: longjdey@126.com
| This article was originally published in a special issue, “Clinical Research in Pharmaceutical and Biomedical Sciences” |
| Indian J Pharm Sci 2021:83(1)spl issue “215-219” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
This study was to investigate and analyze the diagnostic value of nuclear medicine and ultrasound examination in subacute thyroiditis. Three hundred cases with subacute thyroiditis were selected as the research group, while another 300 cases with health examination were enrolled as the control group, both ranging from August 2013 to October 2016. Patients in the research group underwent the detection with erythrocyte sedimentation rate, serum free triiodothyronine, serum free thyroxine, high sensitive thyroid stimulating hormone, thyroid radioactive iodine uptake in 6 h and radionuclide thyroid scan. Patients in both research group and control group took the ultrasound examination. The results of ultrasound examination showed that the thyroid width and thickness in the research group were both significantly larger than those in the control group, revealing statistical significances (p<0.05). The positive rate by nuclear medicine was significantly higher than that by ultrasound examination, revealing p<0.05. Diagnostic positive rate with the combination of nuclear medicine and ultrasound examination was much ideal, that was 100 %. Nuclear medicine and ultrasound examination in subacute thyroiditis could achieve good diagnostic results and provide the accuracy rate of the diagnosis, thus further providing valuable basis for clinical treatment.
Keywords
Nuclear medicine, ultrasound examination, subacute thyroiditis, diagnostic value, observation and investigation
Subacute thyroiditis (SAT) is a self-limiting and non suppurative inflammatory disease in clinic. Still there is no exact theory about its pathogenesis at present. Due to the complicated clinical manifestation of SAT, missed diagnosis and diagnostic errors during the diagnosis often occur. At the same time, together with the high recurrence rate, patient’s body health and living quality are seriously influenced. The survey results of related data have indicated that with the enhancement of people living standard and the changes in life style and dietary habit, patients with SAT gradually reveal a gradually rising tendency, which has aroused wide concerns in the medical field[1].
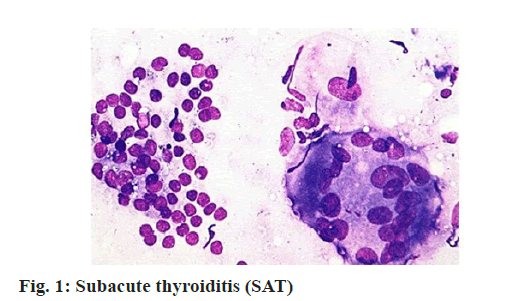
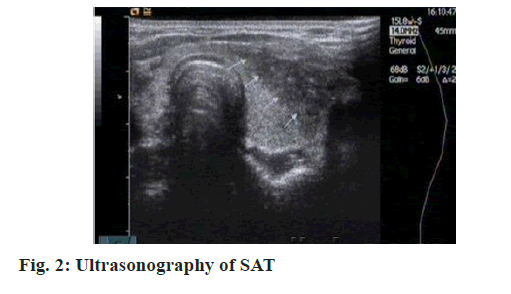
SAT (fig. 1 and fig. 2) is also called as giant cell thyroiditis, mobile thyroiditis and granulomatous thyroiditis, first proposed by De Quervain in 1904[2]. Researches have manifested that there are many pathogens causing SAT, such as coxsackievirus (fig. 3), influenza virus (fig. 4) and echovirus (fig. 5).
With the continuous development of medical career, domestic diagnosis with SAT has also greatly improved in recent years [3-5]. For instance, the application of nuclear medicine is fully embodying the merits of non-invasion, convenience, high sensitivity and high specificity[6,7]. Nuclear medicine combined with ultrasound examination can significantly improve the diagnosis of SAT. Therefore, this study took observation and investigation specific to the diagnostic value of nuclear medicine and ultrasound examination on SAT.
Materials and Methods
General information
Clinical data of 300 cases, who received treatment in our hospital between August 2013 and October 2016 and had confirmed diagnosis by pathological examination, were enrolled as the research group. Those patients included 168 males and 132 females, aged between 24 y and 62 y (average age at (36.7±3.8) y) and disease course ranging from 4 d to 80 d (average disease course of (42.6±2.3) d). All patients were in first episode acute suppurative thyroiditis (AST), with clinical symptoms covering fever, pharyngalgia, hyperhidrosis and weakness. Meanwhile, there were 206 cases with thyroid diffuse enlargement and pain, 125 cases with thyroid nodule enlargement and pain and 289 cases presented as respiratory tract infectious disease history, respectively. As of thyroid involvement, there were 256 cases which involved bilateral sides, 28 cases simply involved right side and 16 cases simply involved left side, respectively. Patients in suckling period or gestation period and with mental disorder and serious organ injury were excluded. Clinical data of 300 cases, who were healthy subjects by examination in our hospital between August 2013 and October 2016, were enrolled as the control group. Those patients included 152 males and 148 females, aged between 22 y and 64 y (average age at (35.8±3.9) years) and excluded neck disease ones. Comparison of data, including ages and genders in the research group and the control group showed comparability, with p>0.05.
Methods
Nuclear medicine and ultrasound examination were applied for patients in the research group and only ultrasound examination for healthy subjects in the control group. Nuclear medicine examination: American customer satisfaction index (ACSI) 80 instrument in chemiluminescence analysis method was used to detect serum free triiodothyronine (FT3), serum free thyroxine (FT4) and high sensitive thyroid stimulating hormone (sTSH)[8]; FH-458 thyroid function device was employed to detect thyroid radioactive iodine uptake in 6 h (RAIU/6 h); Siemens Symbia T single photon emission computed tomography (SPECT) device was adopted for radionuclide thyroid scanning and to take the development at 0.5 h after intravenous infusion of 99Tcm185~259 megabecquerel (MBq)[9]. Development should confirm the following judgment criteria: that without single lobe or double lobe thyroid development in the thyroid site and with clear development in the salivary gland and parotid gland, there was thyroid non development[10,11]; shadow of thyroid gland could be faintly visible, during the time of development of thyroid single lobe or double lobes was relatively prolonged, along with high background, uneven radioactive distribution and clear development in other sites, there was thyroid underdevelopment[12]. Ultrasound examination: SSA-340 color Doppler ultrasonic diagnostic instrument (Toshiba Corporation) was performed for the thyroid ultrasound examination. Patients should keep neck in the supine position and with hyperextension. At the same time, the probe frequency should be controlled in 7.5-10 MHz and local positions of thyroid were scanned in continuous longitudinal and horizon way so as to strictly detect the thyroid thickness and width, regarding anterior cervical muscle and submandibular gland as reference. The detailed record of echo characteristics and the observation of thyroid bleeding were conducted.
Observation indexes
Examination and scan of various indexes for the whole experimental subjects were performed. Comparison between the detected results and normal values were taken. Patients, whose data were not conformed as normal value, they were treated with confirmed diagnosis.
Statistical treatment
SPSS 21.0 statistical software was applied for data analysis, (x±s) for measurement data, (n, %) for enumeration data and t test and Chi square test for intergroup comparison. When p<0.05, it was considered as statistically significant.
Results and Discussion
Patient’s clinical manifestations and laboratory determination results are shown in Table 1. In 300 patients of the research group, there were 145 cases (48.33 %) with positive anti-thyroglobulin antibody (TGA), anti-thyroid microsomal antibody (TMA), 290 cases (96.67 %) with abnormal thyroid γ scintigraphy and 58 cases (19.33 %) with atypical separation between Thyroid hormone (TH) and RAIU, respectively. Moreover, other various indexes were in normal status.
| Items | Symptoms and signs | Examination and test | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Temporary hypothyroidism | Temporary hyperthyroidism | Repeated attack | Premonitory symptom | Fever | Weakness | Thyroid conscious pain | Thyroid enlargement | Positive TGA and TMA | Abnormal thyroid γ scintigraphy | TH and RAIU separation | TH increasing | RAIU obviously decreasing | Increasing erythrocyte sedimentation rate | |
| Cases | 26 | 32 | 40 | 106 | 168 | 100 | 276 | 285 | 145 | 290 | 58 | 156 | 237 | 288 |
| Percentage | 8.67 | 10.67 | 13.33 | 35.33 | 56.00 | 33.33 | 92.00 | 95.00 | 48.33 | 96.67 | 19.33 | 52.00 | 79.00 | 96.00 |
Table 1: Clinical Manifestations and Laboratory Determination Results for Patients in the Research Group (N (%))
Detection results of FT3, FT4 and TSH/sTSH for patients in the research group are shown in Table 2. As indicated in Table 2, in the detection of SAT patients in the research group, there were 268 cases (89.33 %) with hormone changes and 290 cases (96.67 %) with FT3, FT4 and TSH changes. FT3 and TSH were with the highest diagnostic accordance rate, with the sequence of sTSH>FT3>FT4.
| Items | Results data | t | p |
|---|---|---|---|
| FT3 | 6.13±1.22 | -18.36 | <0.05 |
| FT4 | 48.37±4.08 | -29.11 | <0.05 |
| TSH | 0.14±0.06 | 27.13 | <0.05 |
| 6 intake 99mI (%) | 6.95±1.23 | 18.36 | <0.05 |
Table 2: Detection Results of Ft3, Ft4 and Tsh/Stsh For Patients In The Research Group (X±S)
Comparison of ultrasound detection results of thyroid size for patients in both groups is shown in Table 3. As counted, the ultrasound detection results manifested that the thyroid width and thickness for patients in the research group were larger than those for healthy subjects in the control group, with statistical significance (p<0.05). The comparison between the thyroid left and right lobes displayed no significant difference for healthy subjects in the control group, showing p>0.05. Ultrasonic characteristics discovered that all lesions showed hypoechoic dark area, some nearly in anechoic status, irregular border, still clear border, no envelope and neither enhancement effect in posterior wall and posterior nor attenuation or acoustic shadow. Ultrasound detection showed that there were 25 cases with unilateral lesion and 211 cases with bilateral lesion. At the same time, the ultrasound detection rate was 78.67 % (236/300), while the diagnostic rate of nuclear medicine and ultrasound examination was 100 %.
| Group | Cases | Left lobe | Right lobe | ||
|---|---|---|---|---|---|
| Width | Thickness | Width | Thickness | ||
| Research group | 300 | 2.42±0.31 | 2.46±0.43 | 2.32±0.37 | 2.55±0.47 |
| Control group | 300 | 1.11±0.34 | 1.48±0.26 | 1.31±0.35 | 1.21±0.30 |
| t | 25.39 | 20.16 | 22.46 | 19.39 | |
| p | <0.05 | <0.05 | <0.05 | <0.05 | |
Table 3: Comparison of Ultrasound Detection Results of Thyroid Size for Patients in Both Groups (X±S)
As an autoimmune disease, SAT is very common in the thyroid disease, with common age group in 30- 50 y. In accordance with the symptoms, SAT is often involved in acute inflammation period, short recovery period of thyroid function, transient low period of thyroid function and follicle repair period. In the inflammation period, patient’s thyroid follicle (fig. 6) will suffer from extensive destruction, which can lead to thyroid hormone into blood circulation and further cause the rising level of thyroid hormone in the blood. Meanwhile, the destruction of thyroid follicle can also induce the peroxidase dysfunction and the disorder of iodine organification, thus coming into organic iodine by the combination with tyrosine and the decreased ability that is reserved in thyroid follicle, which further emerge low iodine intake rate and decreased thyroid iodine intake ability, as well as the related changes in clinical symptoms.
Ultrasound examination is always regarded as the preferred measure of checking thyroid morphology. The results of ultrasound examination in the two groups suggested that there was no significant difference in the width and thickness of the thyroid left lobe and right lobe in the control group, showing p>0.05. The width and thickness of the thyroid left lobe and right lobe in the research group were significantly larger than those in the control group, showing p<0.05. The typical feature of ultrasound examination of SAT was diffuse enlargement of thyroid single lobe and (or) double lobes. The positive rate of ultrasound detection was 78.67 % (236/300), while the diagnostic rate of nuclear medicine and ultrasound examination was 100 %. Research results indicated that radionuclide scanning combined with ultrasound examination to evaluate thyroid function could significantly enhance the diagnostic rate of SAT.
It was concluded that nuclear medicine and ultrasound examination on SAT could achieve good diagnostic results. Through the evaluation of thyroid function and form, the diagnostic rate could be improved, which was conducive to distinguish and diagnose SAT and other thyroid diseases, thus further providing valuable basis for clinical treatment and effectively inducing the missed diagnosis and diagnostic errors. Therefore, nuclear medicine and ultrasound on SAT deserves application and practices.
Acknowledgements
This work was supported by Jilin Medical and health talents special project (No. 2019SCZT026).
Conflicts of Interest
The authors declared no conflict of interest.
References
- Volta C, Carano N, Street ME, Bernasconi S. Atypical subacute thyroiditis caused by Epstein-Barr virus infection in a three-year-old girl. Thyroid 2005;15(10):1189-91.
- Toda S, Nishimura T, Yamada S, Koike N, Yonemitsu N, Watanabe K, et al. Immunohistochemical expression of growth factors in subacute thyroiditis and their effects on thyroid folliculogenesis and angiogenesis in collagen gel matrix culture. J Pathol 1999;188(4):415-22.
- Volpe R, Johnston MW. Subacute thyroiditis: a disease commonly mistaken for pharyngitis. Can Med Assoc J 1957;77(4):297.
- Tauhata L, Iwahara A, de Oliveira AE, Rezende EA, Delgado JU, da Silva CJ, et al. Proficiency tests in the determination of activity of radionuclides in radiopharmaceutical products measured by nuclear medicine services in 8 y of comparison programmes in Brazil. Appl Radiat Isot 2008;66(6-7):981-7.
- Bailey DL, Roach PJ. A brief history of lung ventilation and perfusion imaging over the 50-year tenure of the editors of Seminars in Nuclear Medicine. Semin Nucl Med 2020;50(1):75-86.
- Lu YJ. Diagnostic value of nuclear medicine and ultrasonography on subacute thyroiditis. China Med Her 2013;11(8):162-6.
- Xu JH, Feng JS. Diagnostic value on subacute thyroiditis with nuclear medicine and ultrasonography. Health 2014;23(11):77.
- Gharbi HA, Hassine W, Brauner MW, Dupuch K. Ultrasound examination of the hydatic liver. Radiology 1981;139(2):459-63.
- Mei F. The Value of nuclear medicine and ultrasonic examination in the diagnosis of subacute thyroiditis. China Foreign Med Treat 2013;10(35):22-3.
- Wang YN, Wang YH, Liu SS, Yan P, Ma SS, Qiu G, et al. Nuclear medicine examination combined ultrasound to evaluate the value of in the diagnosis of subacute thyroiditis. China Health Stand Manag 2016;24(3):164-6.
- Gu Y, Luan X, Ren W, Zhu L, He J. Impact of seasons on stroke-related depression, mediated by vitamin D status. BMC psychiatry. 2018;18(1):1-7.
- Yu XD, Zhang HZ, Chen WX, Zhang YM, Lin ZY. Diagnostic value of nuclear medicine and ultrasonic examination of subacute thyroiditis. Fujian Med J 2016;14(3):117-120.