- *Corresponding Author:
- R. Adepu
Department of Pharmacy Practice, Vikas College of Pharmaceutical Sciences, Rayanigudem, Suryapet, Telangana 508 213, India
E-mail: adepu63@gmail.com
| Date of Received | 12 July 2021 |
| Date of Revision | 17 May 2023 |
| Date of Acceptance | 28 July 2023 |
| Indian J Pharm Sci 2023;85(4):1007-1014 |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
An open label prospective interventional study was conducted on asthma and chronic obstructive pulmonary disease patients to assess the influence of pharmacist provided education on inhaler usage technique and its impact on therapeutic outcomes in patients with Asthma and chronic obstructive pulmonary disease. The study was approved by the institutional ethics committee and conducted in the pulmonology department of Kamineni Institute of Medical Sciences, Narketpalli, Telangana. Written informed consent was obtained from the recruited study patients. A suitably designed data collection form was designed to capture disease and lab details i.e. forced expiratory volume in the 1st second. A newly constructed and validated knowledge, attitude and practices questionnaire was administered to assess the knowledge about the disease and its management. An inhaler checklist was applied to every patient to assess the inhaler usage technique and provided suitable guidance to use the inhaler effectively and assessed the impact of education on the patient's therapeutic outcomes. Among the 20 patients, 11 (55 %) were females and 9 (45 %) were males. The mean age of the study patients was 54±3 y. A significant improvement in knowledge, attitude and practices scores was observed in the post-counselling stage (p<0.001) and inhaler usage technique (p<0.001) among the patient after providing the counselling. Correct education about disease and inhaler usage techniques had shown an improvement in patient ̓s therapeutic outcomes.
Keywords
Asthma, patient counselling, knowledge, attitude and practices, inhaler usage technique
Asthma and Chronic Obstructive Pulmonary Disease (COPD) are chronic respiratory disorders affecting most individuals worldwide leading to the loss of productivity, absence from school and decreased health-related quality of life[1]. Asthma is a chronic inflammatory condition of the airways associated with hyper-responsiveness of the airways and variable airflow obstruction swollen and producing extra mucus, that makes the individual difficult to breathe[2]. In bronchial asthma, a low level of oxygen and a high level of carbon dioxide leads to complications of respiratory failure, pneumonia, and lung collapse (one or both). These complications are mainly due to pulmonary oedema that may cause left heart failure[3].
COPD is a group of lung diseases (emphysema which affects the smaller airways and alveolar sacs, and chronic bronchitis it affects the larger airways are the most common conditions) that block airflow and make it difficult to breathe. Lungs damaged due to COPD cannot be reversed[4]. The major risk factors for COPD are cigarette smoking and long-term exposure to noxious gases and industrial pollutants. In COPD the complications are heart problems, high blood pressure, and lung cancer, depression[5]. Asthma and COPD can be exacerbated when the individual gets exposed to various factors like dust, smoking, air pollution, upper respiratory infections, cold air, occupational exposure, obesity, and family history etc[3].
COPD is the fourth leading cause of death worldwide and it is going to become a third leading cause of death by 2025. In 2001, the World Health Organization (WHO) reported that COPD was the fifth leading cause of death in high-income countries and the sixth leading cause of death in low and middle-income countries. In 2005, an estimated 22.2 million Americans had asthma; 6.5 million children and 15.7 million adults[6]. The public health impact of asthma is significant. In 2003, asthma accounted for 1.4 deaths ̸ 100 000 persons in the USA. According to the National Centre for Health Statistics, in 2003, children between the ages of 5 and 17 y with a history of at least one asthma attack in the previous year accounted for 12.8 million missed school days, and adults with a history of at least one asthma attack in the previous year accounted for 10.1 million missed workdays. The incidence and prevalence rate is high in children when compared to adults, whereas morbidity and mortality are high in adults. The global epidemic status of asthma has been observed in both children and adults, especially in low to middle-income countries. Counselling plays an important role in controlling the disease. Pharmacists could help to bring about disease control by educating the patients about inhalation techniques, taking precautions, diet and some breathing exercises (Pranayama)[5].The inhaler medications constitute short-acting and long-acting beta-2 agonists and steroids that act on beta-2 receptors located in the lungs are used to control the inflammation of bronchi and Leukotriene modifiers are used for managing the allergic reactions[1,3,5].
John Mudge invented the inhaler in 1778 and Pewter Beer Tankard modified the inhaler with a lid. It was operated by using hot water along with opium and the vapours of opium are inhaled for the relief of cough with sputum and other lung problems. Mudge inhalers proved to be more popular and are used to control the inflammation of bronchi and leukotriene modifiers are used for managing the allergic reactions[7]. Modern technologies have modified the inhaler model and improvised it to improve the functioning of the inhaler[8]. To treat allergic asthma, clinical trials in 1970 identified the inhaled corticosteroid intermittent self-dilatation (Beclomethasone dipropionate) in reducing the impact of mast cells, eosinophilic, mononuclear cell inflammation and reversing the late asthmatic reaction. With this, the efficacy in controlling day-to-day life in asthma is improved[9].
Many patients with asthma and COPD are not clear about the correct use of inhalers. This leads to poor control of asthma and COPD. Pharmacists need to educate patients about the disease, precautions, inhaler usage, and medication adherence so that therapeutic outcomes and patient quality of life can be improved[10].
Research studies have corroborated that, patients are often unaware of the correct technique of using the inhaler. This will lead to poor inhalation of the drug and unsatisfactory therapeutic outcomes. Thus, there is a need for training the patients in the proper technique of using inhalers[4]. The life expectancy of individuals get affected by Asthma/COPD can be enhanced by improving their awareness towards the disease, and precautions to take like avoiding exposure to cold air, dust and also avoiding allergic foods, maintaining medication adherence, and correct inhalation usage techniques[11]. Thus, the present study is initiated to assess the inhaler usage technique and train them with an appropriate technique (8-step approach by roger walker) and assess the impact of training of inhaler usage technique on clinical outcomes.
Materials and Methods
The present open-label interventional study was conducted at the pulmonology department, KIMS Hospital, Narketpalli for 6 mo (September 2019-February 2020). The institutional ethical committee has approved the study. The pulmonologists have referred the Asthma/COPD patients using inhalers to the department. Upon explaining the study to the patients meeting the eligibility criteria and willing to give written informed consent and come for the follow-ups were recruited into the study. In this study, patients diagnosed as Asthmatic or with COPD and receiving an inhaler medication. The exclusion criteria are Non-Asthmatic and Non-COPD patients and not receiving an inhaler. A suitable data collection form was used to collect the demographic, clinical and therapeutic data of the enrolled patients at both baseline and final follow-up. Further, a suitably designed Knowledge, Attitude, and Practice (KAP) questionnaire was applied at baseline and the scores were calculated. The patients were given education about the disease, medications, diet and precautions and followed for a period of 1 mo. At the end of 1 mo, once again the KAP questionnaire was re-administered to assess the influence of education on KAP scores. Similarly, at baseline and after one month, an 8-item inhaler checklist was applied. The checklist questionnaire was marked, while the patient was using the inhaler medication about its appropriate usage. Patients were educated subsequently on how good they are using their inhaler medications if any mistakes were found. In order to assess the influence of education on inhaler usage technique and therapeutic outcomes, Forced Expiratory Volume in the 1st s (FEV1) criteria was used and collected the FEV1 scores of all the enrolled patients at baseline and final follow-up.
Data analysis:
Data obtained were analyzed using Statistical Package for the Social Sciences (SPSS) statistical software version. Frequency and statistics were used to analyze the general characteristics of the patients. Data were presented in tables. Student t-test was applied to determine the significance of factors that affected the correct usage of inhaler devices and KAP scores and FEV1 scores. p<0.05 is significant.
Results and Discussion
A total of 20 patients meeting the inclusion and exclusion criteria were recruited. Among them, 8 patients were diagnosed with asthma and 7 patients with COPD and the remaining 5 patients were diagnosed with both asthma and COPD. Many patients were receiving formonide and Combimist-L inhalers compared to other inhalers. Among the study patients, 11 (55 %) were females and 9 (45 %) were males. The mean age of the study patients was 54±3 y. Gender distribution, age distribution, and profession distribution details are presented in Table 1.
| Criteria | Asthma | COPD | Patients with both |
|---|---|---|---|
| Gender | |||
| Male | 0 | 6 | 3 |
| Female | 8 | 1 | 2 |
| Age distribution | |||
| 15-35 y | 3 | 1 | 1 |
| 36-80 y | 5 | 6 | 4 |
| Profession | |||
| Agriculture | 1 | 4 | 3 |
| Labour | 4 | 3 | 2 |
| House wives | 2 | 0 | 0 |
| Students | 1 | 0 | 0 |
| Education | |||
| Illiterate | 5 | 4 | 2 |
| High school | 2 | 2 | 2 |
| Pre-university | 1 | 1 | 1 |
| University | 0 | 0 | 0 |
Table 1: Demographic details of the study patients.
KAP are the qualitative responses taken from the patients towards their understanding of the disease, medicines, and managing the clinical condition. The KAP questionnaire consists of 15 questions. Each question is provided with 4 responses and one is the correct answer. Each correct answer scores one mark. The total score achieved in the pre and post-test is presented in the Table 2.
| KAP Questions | Pre-test Score | Post test | p value |
|---|---|---|---|
| Which part of the body is during COPD/ Asthma? | 18 | 20 | <0.005 |
| Which of the following is a clinical manifestation of Asthma/COPD? | 10 | 17 | <0.005 |
| Which of the following aggravates Asthma? | 12 | 20 | <0.005 |
| Which one of the following leads to COPD? | 6 | 13 | <0.005 |
| Do COPD/ Asthma need long term therapy? | 11 | 20 | <0.005 |
| Whom do you consult, when you experience the severity of COPD/ Asthma? | 18 | 20 | <0.005 |
| Which among these worry you most during an Asthma/ COPD? | 11 | 10 | <0.005 |
| Would you like to take any preventive measures or precautions for Asthma/ COPD? | 7 | 19 | <0.005 |
| What is your response during aggravation of an asthma attack? | 1 | 4 | <0.005 |
| Do you know how to use inhaler? | 9 | 19 | <0.005 |
| What precautions do you take to prevent the re attack of asthma or COPD? | 2 | 12 | <0.005 |
| While using a metered dose inhaler, how frequently the canister should be shaken just before taking a puff? | 3 | 14 | <0.005 |
| In which part of the face, the inhaler should be placed? | 12 | 20 | <0.005 |
| If you are prescribed with steroid inhaler, what do you do while you are using it? | 4 | 13 | <0.005 |
| How often do you consult your doctor? | 10 | 15 | <0.005 |
Table 2: Pre and Post-Test KAP Scores.
In the management of Asthma or COPD, for the improved effect of the medication and decreased adverse effects, Metered Dose Inhalers (MDI) is often being used. An improved therapeutic outcome of the medication depends upon the inhaler usage technique. The inhaler checklist possesses 8 questions to assess how effectively the inhaler is being used by the patient. Each correct answer is awarded 5 marks. The number of correct answers multiplied by 5 is the total score. Details of the total scores before and after the education are presented in Table 3.
| Steps | Baseline score | Final score | p value |
|---|---|---|---|
| 1. Shake the inhaler well | 70 | 95 | <0.006 |
| 2. Remove the dust cap | 75 | 100 | <0.006 |
| 3. Exhale slowly through pursed lips | 60 | 80 | <0.006 |
| 4. Place the inhaler between the lips and close mouth | 45 | 65 | <0.006 |
| 5. Press down on the inhaler once as you start a slow, deep inhalation | 40 | 75 | <0.006 |
| 6. Continue to inhale slowly and deeply through the mouth for at least 5 s | 40 | 50 | <0.006 |
| 7. Hold your breath for 10 s | 45 | 90 | <0.006 |
| 8 Exhale slowly, Wait at least 30-60 s before inhaling the next puff of medicine | 25 | 40 | <0.006 |
Table 3: Pre and Post Test Scores of Inhaler usage check list.
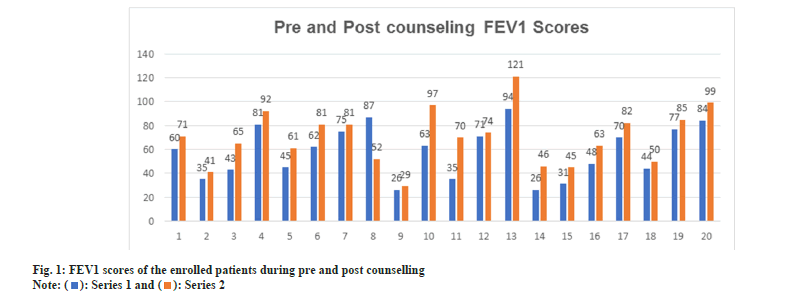
Asthma and COPD patients can estimate their lung capacity by using the Pulmonary Function Test (PFT) and the value of the FEV1. In the pre-test, FEV1 average score was 55.85 in which >80 scored (Mild) by 3 patients, 50-79 scored (Moderate) by 7 patients, 30-49 scored (Severe) by 8 patients and <30 scored (Very severe) were 2 patients. In the post-test (20), the average score was 70.25 in which, >80 scored (Mild) in 8 patients, 50-79 scored (Moderate) in 8 patients, 30-49 scored (Severe) in 3 patients, <30 scored (Very severe) by 1 patient with a statistical significance of <0.001. The details of PFT scores are presented in fig. 1.
COPD are chronic respiratory disorders affecting many individuals worldwide leading to decreased productivity due to absence from school and work. In Asthma, airways become inflamed, narrowed, and swollen and produce extra mucus, which causes difficulty in breathing. COPD is a group of lung diseases (emphysema and chronic bronchitis) that blocks airflow and make it difficult to breathe. Lungs damaged due to COPD cannot be reversed. The main risk factor in COPD is cigarette smoking, and others include long-term exposure to noxious gases and industrial pollutants. In COPD, the complications are heart problems, high blood pressure, and lung cancer, depression. Asthma/COPD can be exacerbated while exposed to factors like dust, smoking, air pollution, upper respiratory infections, cold air, occupational exposure, obesity, family history etc[1].
The success of the treatment depends upon how much the patient is aware of the disease, the precautions to be taken to prevent the triggers and the effective way of using the inhaler. Through education, the patient may be made aware of disease-triggering factors that aggravate the disease condition and proper training to use the inhaler. Using inhaler device medication correctly is an important task for patients suffering from asthma and COPD mainly for illiterate people. But proper education provided by the pharmacist to patients can improve the knowledge towards the disease, and inhaler usage technique and improves patient clinical outcomes[6].
In our study, 20 patients were enrolled. Among them, 9 patients were with asthma, 8 patients were with COPD and 3 patients with both Asthma and COPD. All the patients were using the MDI. The mean age of the patients was 54±3 y. Predominantly asthma cases are seen in females and COPD cases were observed in males. Mainly females are more prone to asthma disease at the age of 19-74. Whereas males are more prone to chronic respiratory diseases such as COPD can occur at the age of 52-75 y.
Age and gender are important factors in the development of respiratory diseases. Currently, bronchial asthma is affecting more than 300 million people worldwide. During childhood, boys have nearly twice the risk of developing asthma over girls but in adulthood, it shifts to female predominance[28]. To assess the influence of age on the precipitation of Asthma, a study was conducted by Maria C M and team through Asthma Call-back Survey in the United States population in 2013. In the study, about 12,216 respondents had given feedback with reference to the age of onset of asthma in them. The findings reveal that the highest incidence was observed during, 1-14 y and 40-50 y of age. In our study, the mean age of the respondents was 53.25 y ranging from 15 to 75 y and the majority of subjects were during the 4th to 6th decade of age. This observation coincides with the findings of Iris Koper’s study[29].
In the study conducted by Koper et al.[29], the observations state that the incidence and severity of asthma are seen higher in women compared to men and especially during the 4th to 6th decade. In assessing the influence of gender on the precipitation of asthma, women report more pronounced symptoms, which seem to change with the various life stages such as menstruation, pregnancy and menopause and in association with female sex hormone levels. These hormones cause differences in the clinical manifestation of asthma. Thus, oestrogen promotes bronchial hyperreactivity, and both FEV1 and exhaled Nitric Oxide (NO) show a cycle-dependent course. Twenty to forty percent (20-40 %) of premenopausal women suffer from Pre or Peri-Menstrual Asthma (PMA) and experience an exacerbation in the week preceding menstruation based on increased inflammation in the bronchi. This effect seems to be mediated by progesterone rather than by oestrogen. PMA is less likely to be associated with atopy, but more frequently with aspirin sensitivity and poor pulmonary function. Currently, the main cause for PMA is considered to be the dynamics or fluctuation rather than the absolute hormone levels, particularly of oestrogen[29].
Tobacco smoking is considered as a major risk factor for COPD, approximately 20 % of smokers develop the disease. The other risk factors responsible for COPD are air pollution, respiratory infections, poor nutritional status, chronic asthma, impaired lung growth, poor socio-economic status and genetic factors. About 15-20 % of COPD cases are due to occupational exposures to pollutants at the workplace, and biomass smoke during lifetime. To assess the prevalence and incidence of COPD by age, sex and smoking status, the Rotterdam Study, a population-based cohort study was conducted with 25 y of follow-up[30]. The study findings suggest that the overall incidence rate of COPD in the Rotterdam Study was approximately 9/1000 per y, with a higher incidence in males and in smokers. The proportion of never smokers among COPD cases is substantial and higher in females than in males.
KAP are very important in successful management of any disease. Prevention of asthma attacks is one of the major challenges of public health. Sufficient knowledge and positive attitudes and correct practices are crucial for the prevention of exacerbations. In our study we educated the patients about how to use an inhaler, knowledge about the disease and lifestyle changes these factors play an important role and showed a high impact on results after the post-test. The pre-counselling KAP score at the baseline was 7.1 and the post-education KAP score was 12.31 (p<0.005). This enhancement was mainly due to education. In a study conducted in Khartoum[31] Sudan to assess the KAP of mothers in controlling the asthma symptoms in their children, the findings suggest that mothers having education in high school or more showed a better understanding of the disease management and symptoms control in their children.
The baseline Inhaler Usage Check List score was 2.1 and after counselling the patients and follow-up, the post-counseling inhaler usage check list score was 5.83 (p<0.005) showing a statistically significant improvement. In our study, the baseline inhaler check list score was found low in the study patients indicating that the patients had poor knowledge about disease and inhaler usage. Proper training for patients and follow-ups shows an improvement in patient inhaler usage. Some studies have shown that structured education for patients may help them to use inhalers correctly. Another study conducted by Kumar et al. [32] studied the influence of pharmacist-provided counselling on disease, medication usage, inhaler usage technique and adherence behaviour on therapeutic outcomes. The study was a randomised control study. A total of 106 patients were distributed in to control (54) and test (52). A validated KAP questionnaire was administered at baseline to assess the pre-education KAP followed by the provision of structured education to test group patients and patients in the control group were casually followed for a period of 1 mo. At the end of the study, a significant improvement was observed in the post-education scores of the patients in the test group. Our study was an open-label study and education was provided to all the patients. Thus, a post-education score was shown significant improvement in all the patients. In the above study, the Inhaler usage checklist was also done along with FEV1 scores. Similar results were observed in the present study indicating the importance of patient education.
Although inhalers are the preferred method of medication delivery, evidence suggests that many patients are unable to use their inhalers effectively due to improper technique so patients must know the right way of their inhaler use. In another study conducted by Shammer et al.[14] with an aim to assess the patient’s ability to use their inhalers properly, identify the most common error made, assess the benefit of single education sessions, compare the property of the use between the primary and secondary clinics patients, determine which type of the inhaler devices is associated with more errors, and to identify the association between the inhaler technique and the disease control. In this non-randomized interventional study using three inhaler types metered-dose inhalers, the inhaler technique was evaluated by a scoring system before and after a single session of training. The results reveal that the current education about inhaler techniques was not sufficient. The response to a single session of education was higher with a high level of education, urban area, and specialized respiratory centre. Better disease control with a better score. After training, the younger patients have a higher score. The authors have concluded the study the patients need more training and single class of training can be beneficial but need follow-up to see if this effect need to be maintained.
Similar findings were also observed in another study conducted by Shrestha et al.[15] and her colleagues on inhaled medication usage in COPD patients. The researchers assessed and trained on the inhaler technique through video demonstration. 8 item inhaler checklist was employed at baseline and the final follow-up after 3 mo. The final findings suggest that the mean percentage of pre counselling score was 44.43 % and the post counselling score was 86.4 % with a statistically significant improvement. Relatively poor technique and best technique were seen at baseline and immediately after counselling respectively which slightly deteriorated after 2 w. Regular counselling and assessment with suitable teaching aids can improve the inhalation technique of COPD patients.
In the present study, the pre-counselling pulmonary function test, FEV1 score was 55.85 and the final follow-up score was 70.25 showing a statistically significant improvement. This suggests the influence of counselling on inhaler usage technique, which significantly improved the therapeutic outcomes and thereby the clinical outcomes. Similar findings were demonstrated in study by Kumar et al.[32].
All the findings have shown a positive impact of counselling on KAP scores, inhaler usage technique and FEV1 scores. In our study, the majority of patients with asthma and COPD were illiterate and do not know how to use an inhaler correctly. Therefore, pharmacist education and care for patients is an important step to minimize disease progression and improve symptom control and health-related quality of life. The study findings demonstrated the same in our study.
Conflict of interests:
The authors declared no conflict of interests.
References
- Cruz AA. Global surveillance, prevention and control of chronic respiratory diseases: A comprehensive approach. World Health Organization; 2007.
- Global Initiative for Asthma Executive Committee. Global strategy for asthma management and prevention (revised 2002). In: NHLBI/WHO Workshop Report; 2006.
- Zelalem BK, Mamo G, Feiysa D. Effect of intervention on metered dose inhaler use technique and determinants among adult asthmatic patients attending in outpatient clinic, Ethiopia: Interventional study. Int J Respir Pulm Med 2020;7:136.
- Reema T, Adepu R, Sabin T. Impact of clinical pharmacist intervention on knowledge, attitude and practice (KAP) of patients with chronic obstructive pulmonary disease. Age (Yrs) 2010;61:13-5.
- Molimard M, Raherison C, Lignot S, Balestra A, Lamarque S, Chartier A, et al. Chronic obstructive pulmonary disease exacerbation and inhaler device handling: Real-life assessment of 2935 patients. Eur Respir J 2017;49(2).
[Crossref] [Google Scholar] [PubMed]
- Sinha B, Singla R, Chowdhury R. An epidemiological profile of chronic obstructive pulmonary disease: a community-based study in Delhi. J postgrad med 2017;63(1):29.
[Crossref] [Google Scholar] [PubMed]
- Salvi S, Kumar GA, Dhaliwal RS, Paulson K, Agrawal A, Koul PA, et al. The burden of chronic respiratory diseases and their heterogeneity across the states of India: The Global Burden of Disease Study 1990–2016. Lancet Glob Health 2018;6(12):e1363-74.
[Crossref] [Google Scholar] [PubMed]
- Ganguly A, Das AK, Roy A, Adhikari A, Banerjee J, Sen S. Study of proper use of inhalational devices by bronchial asthma or COPD patients attending a tertiary care hospital. J Clin Diagn Res 2014;8(10):HC04.
[Crossref] [Google Scholar] [PubMed]
- McGeachie MJ. Childhood asthma is a risk factor for the development of chronic obstructive pulmonary disease. Curr Opin Allergy Clin Immunol 2017;17(2):104.
[Crossref] [Google Scholar] [PubMed]
- Farabaugh N, McMillan A, Garofoli G. Assessment of asthma inhaler technique in two community pharmacies. Innov Pharm 2014;5(3):1-7.
- Holgate ST. A brief history of asthma and its mechanisms to modern concepts of disease pathogenesis. Allergy Asthma Immunol Res 2010;2(3):165-71.
[Crossref] [Google Scholar] [PubMed]
- Batterink J, Dahri K, Aulakh A, Rempel C. Evaluation of the use of inhaled medications by hospital inpatients with chronic obstructive pulmonary disease. Can J Hosp Pharm 2012;65(2):111.
[Crossref] [Google Scholar] [PubMed]
- Walker R. Clinical pharmacy and therapeutics E-Book. Elsevier Health Sciences; 2011:425.
- Shammer NH, Baay AS. Assessment of inhalers technique proper use for patients with chronic respiratory diseases in primary and secondary clinics in Babylon city. Asian J Pharm Clin Res 2018;11(3)-199.
- Shrestha S, Sapkota B, Ghimirey A, Shakya R. Impact of counseling in inhalation technique (rotahaler) in chronic obstructive pulmonary disease patients. Int J Pharm 2013;3(3):442-9.
- E. Hesselink, Brenda WJH Penninx, Hanneke AH Wijnhoven, Didi MW Kriegsman, Jacques TM van Eijk A. Determinants of an incorrect inhalation technique in patients with asthma or COPD. Scand J Prim Health Care 2001;19(4):255-60.
[Crossref] [Google Scholar] [PubMed]
- Suthar J, Patel ZA, Shelat B. Assessment of inhalation techniques in COPD and asthma patients using metered dose inhaler and rota-haler. Indian J Pharm Pract 2019;12(4).
- Al-Jahdali H, Ahmed A, Al-Harbi A, Khan M, Baharoon S, Salih SB, et al. Improper inhaler technique is associated with poor asthma control and frequent emergency department visits. Allergy Asthma Clin Immunol 2013;9:1-7.
[Crossref] [Google Scholar] [PubMed]
- Onyedum CC, Desalu OO, Nwosu NI, Chukwuka CJ, Ukwaja KN, Ezeudo C. Evaluation of inhaler techniques among asthma patients seen in Nigeria: An observational cross sectional study. Ann Med Health Sci Res 2014;4(1):67-73.
[Google Scholar] [PubMed]
- Yildiz F, Asthma Inhaler Treatment Study Group. Importance of inhaler device use status in the control of asthma in adults: The asthma inhaler treatment study. Respir Care 2014;59(2):223-30.
[Crossref] [Google Scholar] [PubMed]
- Pothirat C, Chaiwong W, Phetsuk N, Pisalthanapuna S, Chetsadaphan N, Choomuang W. Evaluating inhaler use technique in COPD patients. Int J Chron Obstruct Pulmon Dis 2015:1291-8.
[Crossref] [Google Scholar] [PubMed]
- Sriram KB, Percival M. Suboptimal inhaler medication adherence and incorrect technique are common among chronic obstructive pulmonary disease patients. Chron Respir Dis 2016;13(1):13-22.
[Crossref] [Google Scholar] [PubMed]
- Chogtu B, Holla S, Magazine R, Kamath A. Evaluation of relationship of inhaler technique with asthma control and quality of life. Indian J Pharmacol 2017;49(1):110.
[Google Scholar] [PubMed]
- Gregoriano C, Dieterle T, Breitenstein AL, Dürr S, Baum A, Maier S, et al. Use and inhalation technique of inhaled medication in patients with asthma and COPD: Data from a randomized controlled trial. Respir Res 2018;19(1):1-5.
[Crossref] [Google Scholar] [PubMed]
- Al-Worafi YM. Evaluation of inhaler technique among patients with asthma and COPD in Yemen. J Taibah Univ Med Sci 2018;13(5):488-90.
[Crossref] [Google Scholar] [PubMed]
- Samady W, Rodriguez VA, Gupta R, Palac H, Karamanis M, Press VG. Critical errors in inhaler technique among children hospitalized with asthma. J Hosp Med 2019;14(6):361-5.
[Crossref] [Google Scholar] [PubMed]
- Carey MA, Card JW, Voltz JW, Arbes SJ, Germolec DR, Korach KS, et al. It's all about sex: gender, lung development and lung disease. Trends Endocrinol Metab 2007;18(8):308-13.
[Crossref] [Google Scholar] [PubMed]
- Mirabelli MC, Beavers SF, Chatterjee AB, Moorman JE. Age at asthma onset and subsequent asthma outcomes among adults with active asthma. Respir Med 2013;107(12):1829-36.
[Crossref] [Google Scholar] [PubMed]
- Koper I, Hufnagl K, Ehmann R. Gender aspects and influence of hormones on bronchial asthma–Secondary publication and update. World Allergy Organ J 2017;10:46.
[Crossref] [Google Scholar] [PubMed]
- Terzikhan N, Verhamme KM, Hofman A, Stricker BH, Brusselle GG, Lahousse L. Prevalence and incidence of COPD in smokers and non-smokers: The Rotterdam Study. Eur J Epidemiol 2016;31:785-92.
[Crossref] [Google Scholar] [PubMed]
- Ahmed Abdulgadir Noureddin, Ahmed Ali Abdalla et al. The knowledge attitude and practice (KAP) of mothers of Asthmatic children towards Asthma in Khartoum Asthma clinics Scientific Reports. Sci Rep 2019;9:121.
- Kumar DSA, Adepu R, Parthasarathi G, Mahesh PA. Impact of community pharmacist provided patient education in asthma patients on treatment outcomes: A Study. Indian J Pharm Edu 2009;43(2):125-133.
 .
.



