- *Corresponding Author:
- Xia Chen
Department of Gastroenterology, Zhongda Hospital, School of Medicine, Southeast University, No.87, Dingjiaqiao Road, Gulou District, Nanjing, 210009, Jiangsu, China
E-mail: chenxia19780125@163.com
| This article was originally published in a special issue, “Therapeutic Perspectives in Biomedical Research and Pharmaceutical Sciences and their Nursing Methods” |
| Indian J Pharm Sci 2021:83(4)spl issue “50-55” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
A total of 98 patients with choledocholithiasis admitted to our hospital from February 2019 to February 2020 were selected. All the patients were divided into the observation group (n=49) and the control group (n=49) according to random number method. The operative time, drainage tube retention time, first anal exhaust time and hospital stay were compared between the two groups. The pain of the two groups was compared at 1st d, 3rd d and 7th d after operation. The incidence of pancreatitis, cholangitis, infection, bleeding and hyperamylasemia and the satisfaction of patients with nursing were compared between the two groups after operation. Compared with the control group, the success rate of lithotomy in the observation group was significantly increased (p<0.05). The operation time, drainage tube retention time, first anal exhaust time and hospitalization time in observation group were significantly lower than those in control group (p<0.05). Compared with the control group, the pain degree of observation group at 1st d, 3rd d and 7th d after surgery was significantly decreased (p<0.05). In addition, the incidence of postoperative complications in observation group was significantly decreased (p<0.05) and nursing satisfaction was significantly increased (p<0.05). The operation cooperation and clinical nursing for patients with choledocholithiasis treated with non-ray endoscopic retrograde cholangiopancreatography can significantly improve the success rate of operation, reduce the injury caused by operation and improve the prognosis of patients, which has high clinical application value.
Keywords
Choledocholithiasis, gallbladder, lithotomy, endoscopic retrograde cholangiopancreatography
Choledocholithiasis is clinically high in incidence. According to the sources, choledocholithiasis can be divided into primary choledocholithiasis and secondary choledocholithiasis from gallbladder [1]. Pathological studies showed that [2], the severity of patients with choledocholithiasis and the clinical manifestations may be related with the degree of stone obstruction and the occurrence of biliary tract infection. Due to bile retention, dilatation of common bile duct, contraction of gallbladder and peristalsis of common bile duct, stones can be displaced or eliminated. When the obstruction is removed, the bile retention is also relieved [3]. However, once biliary tract infection worsens, acute obstructive suppurative cholangitis also appears at this time, and the disease develops rapidly. In this case, more patients will suffer from adverse reactions such as dysphoria, coma and blood pressure drop. If they are not treated in time, the patients will eventually die due to circulatory failure [4]. In the past, the main treatment methods for choledocholithiasis included cholecystectomy and common bile duct exploration combined with T-tube drainage. However, long-term clinical experiments have indicated that the modified indwelling T-tube will cause bile loss and electrolyte imbalance of patients and improper nursing of T-tube will cause adverse phenomena such as catheter displacement and slippage, seriously affecting the therapeutic effect and quality of life of patients [5]. In recent years, with the continuous improvement of medical technology, endoscopic retrograde cholangiopancreatography (ERCP) has become a common stone removal method for clinical treatment of choledocholithiasis. It has advantages of simple operation, few complications and good prognosis [6]. Although this technique is relatively mature, the disease is easy to relapse after operation that requires multiple stone removal, thus exerting adverse effects on patients [7]. Therefore, preoperative, intraoperative and postoperative nursing is of great significance. In this study, the intraoperative cooperation and clinical nursing countermeasures of non-ray ERCP in the treatment of patients with choledocholithiasis will be investigated, aiming at improving the curative effect of clinical treatment of choledocholithiasis and the prognosis of patients. It was reported as follows.
Materials and Methods
General data:
A total of 98 patients with choledocholithiasis admitted to our hospital from February 2019 to February 2020 were selected, including 62 males and 36 females, aged 25~60 y old, with an average age of 31.05±3.29 y old, with a course of 1~5 y and an average course of 2.59±0.62 y. Among them, there were 61 cases of single stone and 37 cases of multiple stones. Education level: 16 cases in primary school, 24 cases in junior high school, 19 cases in senior high school, 20 cases in junior college and 19 cases with bachelor degree or above. All patients were randomly divided into the observation group and the control group, with 49 cases in each group. All patients and their families were aware of this study and have signed informed consent forms.
Inclusion criteria and exclusion criteria:
Inclusion criteria-patients with complete clinical data; patients diagnosed as choledocholithiasis by B-ultrasound, Computed tomography (CT) or magnetic resonance; patients who can tolerate ERCP; non-pregnant or lactating women; patients who meet the indications of ERCP. Exclusion criteria-patients with severe heart, liver and kidney dysfunction; patients with mental disorders; patients who cannot communicate with medical personnel; patients with serious autoimmune systemic diseases; patients who have undergone catheterization recently.
Surgical methods:
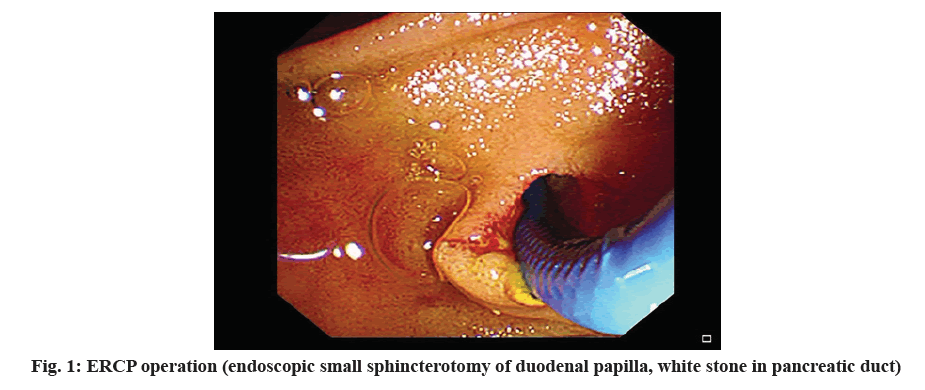
All patients underwent ERCP in the lateral position. The medical staff placed the left arm of the patient behind him, used duodenoscope to find the position of the large duodenal papilla of the patient, then incised the duodenal papilla of the patient through biopsy channel, inserted the guide wire into the common bile duct of the patient, injected iohexol contrast agent into it and performed cholangiography. Through cholangiography, we can know the specific location, size and number of common bile duct stones of patients and then take stones. The nasobiliary duct in the middle is drained by stone removal gas. Under the action of endoscope, it is inserted into the common bile duct in the middle and the other end is led out from the duodenum, stomach, esophagus and pharynx of the patient to the nostril of the patient for bile drainage in vitro. In the drainage process, the traditional Chinese medicine is ensured to be carried out under the condition of sterility and the nasobiliary duct is removed after the choledocholithotomy of the patient is completed. The number of times of stone removal depends on the patients’ physical condition.
Intraoperative cooperation and nursing methods:
Patients in the observation group were given intraoperative cooperation and clinical nursing. Patients in the control group were given conventional nursing.
Preoperative nursing: Medical staff should first have a comprehensive understanding of the patients’ clinical data, including the surgical history, allergy history, etc. They should tell patients and their families about the operation process and key points of cooperation. The cardiopulmonary function and coagulation function of the patient will be tested and the finger pulse oxygen of the patient in prone position should be more than 95 %. Medical staff will prepare all the articles, medicines and instruments needed during the operation before the operation, guide the patients’ diet and fasting time before operation and tell the patient about the successful cases, so as to enhance the confidence of the patient in overcoming the disease.
Intraoperative cooperation: During the operation, the medical staff should help the patient to take prone position to keep his breathing unobstructed. During the operation, the nursing staff sent a tentative and gentle insertion guide wire according to the doctor’s requirements and adjusted the direction appropriately when the resistance was large. Before iohexol is injected, air should be exhausted to prevent the contrast results from being affected. Nursing staff should pay attention to the tightness of the steel wire of the cutting knife. Too tight will cause the cutting knife to be unable to move forward and local electrocoagulation will occur. Small stones can be taken out directly, while larger rocks need to be taken out after mechanical crushing. When the patient undergoes surgery, the nursing staff should always observe the emotional state of the patient, give effective help to the patient, stabilize the patients’ mood, patiently communicate with the patient and relieve his nervous mood. During the operation, changes in the patients’ vital signs should be detected at any time. In case of any abnormal situation, the doctor should be informed in time for further treatment.
Postoperative nursing: After the operation, the nursing staff will help the patients to be sent to the ward with doctors and make a good connection with the nurses in the ward. The related staff will tell the patients about the matters needing attention after operation, give them electrocardiogram (ECG) monitoring, oxygen inhalation, monitor the patients’ vital signs and know whether the patients have any adverse reactions. In addition, the drainage tube should be treated well to ensure that it remains unobstructed and sterile and the color and drainage volume of the drainage tube should be recorded.
Observation index:
Success rate of stone removal-The success rate of stone removal between the two groups was compared; Operation conditions-The operation time, drainage tube retention time, anal first exhaust time and hospitalization time of the two groups were compared; Pain level-Visual analogue scale (VAS) was used to compare the pain of the two groups on the 1st, 3rd and 7th d after operation; Complications and nursing satisfaction-The incidence of pancreatitis, cholangitis, infection, hemorrhage and hyperamylasemia after operation and the satisfaction of patients with nursing were compared between the two groups. Nursing satisfaction was divided into very satisfied, satisfied and dissatisfied. Satisfaction rate= (very satisfied+satisfied)/total number of cases.
Statistical processing:
Statistical package for the social sciences (SPSS) 22.0 statistical software was used to analyze the data. The measurement data conforming to normal distribution were expressed as mean±standard deviation (x̄±s) and the comparison between groups was conducted by T test; Counting data were expressed as the number of cases (n) or percentage (%) and the data comparison was tested by χ2 test. When p<0.05, the difference was statistically significant.
Results and Discussion
There were no significant differences in gender, average age, average course of disease, Body mass index (BMI), stone type and educational level between the two groups (p>0.05), as shown in Table 1.
| Group | Observation group (n=49) | Control group (n=49) | Statistical value | P value | |
|---|---|---|---|---|---|
| Gender (case) | Male | 30 | 32 | 5.267 | 0.492 |
| Female | 19 | 17 | |||
| Mean age (y old) | 30.15±2.07 | 31.06±2.05 | 4.269 | 1.003 | |
| Mean duration of disease (d) | 2.56±0.59 | 2.67±0.64 | 6.238 | 0.068 | |
| BMI (kg/m2) | 22.05±3.20 | 22.46±3.07 | 4.198 | 0.129 | |
| Types of stones (cases) | Single stone | 30 | 31 | 5.220 | 0.218 |
| Multiple stone | 19 | 18 | |||
| Education level (cases) | Primary school | 8 | 8 | 5.267 | 0.459 |
| Junior high school | 12 | 12 | |||
| High school | 9 | 10 | |||
| Junior college | 10 | 10 | |||
| Bachelor degree or above | 10 | 9 | |||
Table 1: Comparison of General Data Between the Two Groups
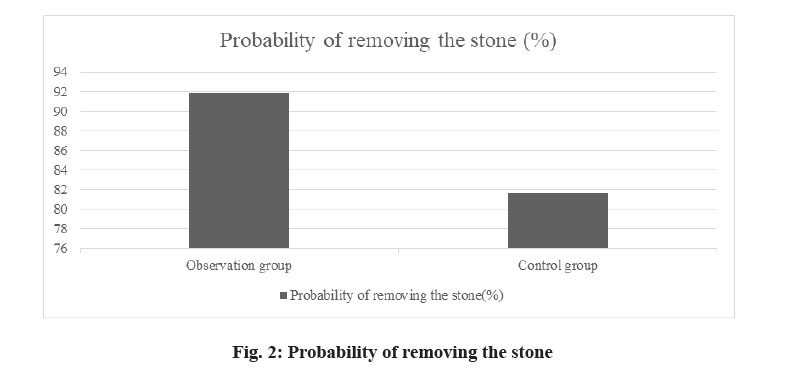
In the observation group, the stones were successfully removed from 45 cases and the stone removal rate was 91.83 %. There were 40 cases of successful stone removal in the control group and the stone removal rate was 81.63 %. The stone removal rate of patients in the observation group was significantly higher than that in the control group and the difference was statistically significant (p<0.05), see fig. 1 and fig. 2.
The operation time, drainage tube retention time, anal first exhaust time and hospitalization time of patients in the observation group were significantly lower than those in the control group and the differences were statistically significant (p<0.05), see Table 2.
| Group | Observation group (n=49) | Control group (n=49) | T value | P value |
|---|---|---|---|---|
| Operation time (min) | 95.02±10.02 | 115.26±10.48 | 5.269 | 0.005 |
| Drainage tube retention time (h) | 50.14±5.20 | 68.59±5.26 | 6.318 | 0.015 |
| First exhaust time (h) | 30.48±3.20 | 50.03±7.26 | 6.004 | 0.026 |
| Length of stay (d) | 8.20±1.05 | 11.86±3.29 | 5.228 | 0.009 |
Table 2: Comparison of Surgical Conditions Between the Two Groups
The pain degree of patients in the observation group was significantly lower than that in the control group at 1st d, 3rd d and 7th d after operation and the differences were statistically significant (p<0.05), see Table 3.
| Group | Observation group (n=49) | Control group (n=49) | T value | P value |
|---|---|---|---|---|
| 1 d after operation | 3.48±1.03 | 4.66±1.02 | 5.269 | 0.005 |
| 3 d after operation | 2.51±1.02 | 3.26±1.08 | 6.318 | 0.015 |
| 7 d after operation | 2.10±0.48 | 2.85±0.62 | 6.004 | 0.026 |
Table 3: Comparison of Pain Between the Two Groups (x̄±s, Point)
The incidence of postoperative complications in the observation group was significantly lower than that in the control group, while the nursing satisfaction of patients in the observation group was significantly higher than that in the control group and the differences were statistically significant (p<0.05), see Table 4.
| Group | Observation group (n=49) | Control group (n=49) | T value | P value |
|---|---|---|---|---|
| Pancreatitis | 1 (2.04) | 1 (2.04) | 5.269 | 0.005 |
| Cholangitis | 1 (2.04) | 2 (4.08) | ||
| Infection | 0 (0.00) | 2 (4.08) | ||
| Bleeding | 1 (2.04) | 1 (2.04) | ||
| Hyperamylasemia | 0 (0.00) | 2 (4.08) | ||
| Total occurrence | 3 (6.12) | 8 (16.32) | ||
| Very satisfied | 20 (40.81) | 18 (36.73) | 5.789 | 0.002 |
| Satisfied | 27 (55.10) | 23 (46.93) | ||
| Not satisfied | 2 (4.08) | 8 (16.32) | ||
| Satisfaction | 47 (95.91) | 41 (83.67) |
Table 4: Comparison of Complications and Nursing Satisfaction Between the Two Groups [n (%)]
The choledocholithiasis is common clinically. Due to the obstruction caused by stones, the pathogenesis of patients is complex and diversified [8]. According to clinical research [9], the main clinical manifestations of patients with choledocholithiasis include abdominal pain, jaundice, etc. The patients with choledocholithiasis will have liver seriously damaged, which may develop into other diseases. Therefore, the targeted treatment is of vital importance to the life safety of patients affected. ERCP has been widely used in clinic at present. It has the advantages of fewer traumas, short operation time and fewer complications. Compared with conventional surgery, ERCP not only reduces the economic pressure of patients, but also reduces the damage caused by surgery to patients [10-11]. However, some related studies have found [12] that some patients with choledocholithiasis undergoing ERCP had a low awareness of ERCP, a poor compliance with treatment and serious negative emotions. Therefore, it is particularly important to take certain nursing measures for patients.
Radadiya et al. [13] found that the stone removal rate can reach more than 85 % by cooperation and nursing on patients undergoing ERCP. Asenov et al. [14] also found that after nursing, the compliance of patients with ERCP was significantly improved. In the above study, it was found that the success rate of stone removal in the observation group was significantly higher than that in the control group, which indicated that intraoperative cooperation and clinical nursing could significantly improve the curative effect of ERCP operation. This may be related to keeping the patient in the optimal condition during the operation, which is consistent with the research results of many scholars mentioned above. Min et al. [15] found that the ERCP is not only related to the operation method, but also closely related to the nursing method. The research results of Duan Guanyu and others [16] showed that cooperating with doctors during ERCP can promote the smooth completion of the operation and shorten the operation time. Lyu et al. [17] told us that the hospitalization time of patients with choledocholithiasis with all-round nursing is significantly reduced compared with that of patients with choledocholithiasis undergoing routine nursing. In the above study, the operation time, drainage tube retention time, anal first exhaust time and hospitalization time of patients in the observation group were significantly lower than those in the control group. It was suggested that intraoperative cooperation and clinical nursing for patients with choledocholithiasis undergoing radiationfree ERCP can significantly improve the operation situation and reduce the pain caused by the operation. The reason may be that the operation was optimized during the operation to avoid the occurrence of adverse reactions, thus shortening the operation time and the retention time of drainage tube and promoting the recovery of patients. This is consistent with the research results of many scholars mentioned above. In the above study, VAS was used to evaluate the pain degree in different time periods. The results showed that the pain degree of the observation group was significantly lower than that of the control group in each time period. To a certain extent, intraoperative cooperation and nursing can significantly reduce the pain of patients and relieve the clinical discomfort of patients. This is consistent with the results of Ning et al. [18] in the research on nursing of patients with choledocholithiasis undergoing ERCP. The above study also found that the incidence of postoperative complications in the observation group was significantly lower than that in the control group, while the nursing satisfaction of patients in the observation group was significantly higher than that in the control group. Based on this, the cooperation and nursing during ERCP can improve the prognosis of patients with choledocholithiasis and improve the doctor-patient relationship. This may be due to calming the patient’s mood during the operation so that they can try their best to cooperate with the operation and help the patient recover after the operation. This is consistent with the research results of Wang et al. [19] and Yadong et al. [20]
To sum up, in the treatment of choledocholithiasis with ERCP, effective intraoperative cooperation and preoperative and postoperative nursing can promote the smooth completion of the operation, reduce the occurrence of postoperative complications of patients and improve their quality of life, which has high clinical value.
Acknowledgements:
None.
Conflicts of interest:
The authors report no conflicts of interest.
References
- Buxbaum JL, Fehmi SM, Sultan S, Fishman DS, Qumseya BJ, Cortessis VK, et al. ASGE guideline on the role of endoscopy in the evaluation and management of choledocholithiasis. Gastrointest Endosc 2019;89(6):1075-105.
- Frybova B, Drabek J, Lochmannova J, Douda L, Hlava S, Zemkova D, et al. Cholelithiasis and choledocholithiasis in children; risk factors for development. PLoS One 2018;038(005):479-82.
- Parra-Membrives P, Martínez-Baena D, Lorente-Herce JM, Jiménez-Riera G, Sánchez-Gálvez MÁ. Choledocholithiasis recurrence following laparoscopic common bile duct exploration. Cir Esp 2019;97(6):336-42.
- Pang WX, Jiang HC. Research progress in surgical treatment of common bile duct stones. Int J Surg 2021;8(5):29-37.
- Lin H, Cheng R, Chen Y. Comparison of minimally invasive surgery and laparotomy for patients with cholecystolithiasis and common bile duct stones. Chin J Pract Diagn Treatment 2019;8(2):56-66.
- Wang Z, Zhu L. Research progress on prevention and treatment of complications after endoscopic retrograde cholangiopancreatography. Chin J Pract Int Med 2019;9(1):33-40.
- Ng DY, Petrushnko W, Kelly MD. Clip as nidus for choledocholithiasis after cholecystectomy-literature review. JSLS 2020;24(1):e2019.00053.
- Chisholm PR, Patel AH, Law RJ, Schulman AR, Bedi AO, Kwon RS, et al. Preoperative predictors of choledocholithiasis in patients presenting with acute calculous cholecystitis. Gastrointest Endosc 2019;89(5):977-83.
- Somasekar K, Chan DS, Sreekumar NS, Anwer S. Choledocholithiasis after bariatric surgery—more than a stone’s throw to reach?. J Gastrointest Surg 2018;22(3):529-37.
- Pan L, Chen M, Ji L, Zheng L, Yan P, Fang J, et al. The safety and efficacy of laparoscopic common bile duct exploration combined with cholecystectomy for the management of cholecysto-choledocholithiasis: an up-to-date meta-analysis. Ann Surg 2018;268(2):247-53.
- Xu Y, Dongjun A, Yang W. Clinical study on different surgical schemes for cholecystolithiasis complicated with common bile duct stones. J Laparosc Surg 2019;8(8):28-30.
- Zhang D, Tang X, Xu C. A large sample study of endoscopic retrograde cholangiopancreatography in children with biliary and pancreatic diseases. J Laparosc Surg 2019;27(2):308-312.
- Radadiya D, Devani K, Arora S, Charilaou P, Brahmbhatt B, Young M, et al. Peri-procedural aggressive hydration for post endoscopic retrograde cholangiopancreatography (ERCP) pancreatitis prophylaxsis: meta-analysis of randomized controlled trials. Pancreatology 2019;19(6):819-27.
- Asenov Y, Akın M, Cantez S, Soysal FG, Tekant Y. Endoscopic retrograde cholangiopancreatography in children: Retrospective series with a long-term follow-up and literature review. Turk J Gastroenterol 2019;30(2):192.
- Ma M, Zhou Z. Comparative observation of acute pancreatitis and hyperamylasemia after endoscopic retrograde cholangiopancreatography. J Clin Hepatobiliary Dis 2020;12(7):174-84.
- Duan G, He X. Application progress of endoscopic retrograde cholangiopancreatography in the diagnosis and treatment of common bile duct stones. J Clin Dig Dis 2020;8(21):7-20.
- Lyu Y, Cheng Y, Li T, Cheng B, Jin X. Laparoscopic common bile duct exploration plus cholecystectomy versus endoscopic retrograde cholangiopancreatography plus laparoscopic cholecystectomy for cholecystocholedocholithiasis: a meta-analysis. Surg Endosc 2019;33(10):3275-86.
- Xue N, Lei X, Xu J, et al. Application progress of endoscopic retrograde cholangiopancreatography in children with pancreatic and biliary diseases. Chin J Pediatr 2021;16(31):46-51.
- Wang TJ, Ryou M. Evolving techniques for endoscopic retrograde cholangiopancreatography in gastric bypass patients. Curr Opin Gastroenterol 2018;8(32):68-70.
- Laiya D, Zhuang H, Shuhui L. Application value of endoscopic retrograde cholangiopancreatography in benign duodenal stenosis complicated with common bile duct stones. Chinese Journal of Digestive Endoscopy 2020;28(12):2211-3.