- *Corresponding Author:
- Majed H Wakid
Department of Medical Laboratory Sciences, Faculty of Applied Medical Sciences, King Abdulaziz University, Jeddah, Saudi Arabia
E-mail: mwakid@kau.edu.sa
| Date of Received | 11 March 2025 |
| Date of Revision | 13 March 2025 |
| Date of Accepted | 30 March 2025 |
| Indian J Pharm Sci 2025;87(2):52-58 |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
Toxoplasma gondii is a protozoan intracellular obligate parasite found worldwide and cause Toxoplasmosis. The Kingdom of Saudi Arabia is at the forefront of countries that are exposed to traffic accidents, in addition to losing people, and it is also an economic issue that has cost the government huge sums of money. The main objective of the current study was to explore the relationship between latent toxoplasmosis and traffic accidents among Saudi male drivers. A case-control study was conducted to clarify the main aim of the study. Data were collected from the experimental and control group after signing the consent form using a questionnaire. Blood samples were collected from each participant and immunoglobulin G and immunoglobulin M enzyme-linked immunosorbent assay were used to differentiate between acute and latent infection. The prevalence of chronic toxoplasmosis immunoglobulin G in the current study was 23.8 % in drivers with a traffic accident history. The results obtained in this study indicate that the traffic accident may be due to chronic toxoplasmosis infection (p<0.009). The results obtained showed that cutting raw meat without wearing gloves may be the main source of chronic toxoplasmosis infection (p<0.05). The result showed that retired people were more susceptible to infection compared to other groups (p<0.05). The current study confirmed the relationship between chronic toxoplasmosis infection and traffic accidents, and the source of the infection was determined. Therefore, to avoid the consequences of public health and economic underestimation, we recommend linking the issuing of the traffic license with a negative result for chronic toxoplasmosis.
Keywords
Latent toxoplasmosis, Toxoplasma gondii, traffic accident, immunoglobulin G detection
Toxoplasmosis is a disease caused by an obligate intracellular protozoan called Toxoplasma gondii (T. gondii). The main routes of infection occurred through consumption of raw or undercooked meat containing bradyzoites, as well as vegetables or fruits contaminated with the oocysts. Vertical or congenital transmission can also occur from a pregnant mother to her fetus once the primary infection is transmitted early during pregnancy. Transmission can occur via blood transfusion and organ transplantation[1,2]. After a brief infection with the acute phase of T. gondii, the infection progresses to latent toxoplasmosis when tachyzoites transform to bradyzoites and reside mainly in the nervous system or muscle tissue throughout the life of the host. Reactivation of bradyzoites and retransformation to tachyzoites may also occur particularly in immunosuppressed individuals. Latent infection is usually asymptomatic, but may also cause pneumonia, myocarditis, chorioretinitis, and fatal encephalitis[3,4].
After a recent T. gondii infection, the parasite may lie dormant in the brain and muscles of infected people without any known symptoms. This phenomenon is called latent toxoplasmosis. Several studies have been conducted in different countries in different groups to explore the effectiveness of latent infection in people and especially on personality characteristics or behaviour. These studies related latent toxoplasmosis with several conditions such as schizophrenia, Parkinson’s disease, inspirations of personality and behaviour of human, impairs psychomotor performance, enhancement of suicide, traffic accident, and the birth of male offspring[5-15]. In addition, men with latent toxoplasmosis were found to be more likely to ignore rules, more expedient, jealous, suspicious, and dogmatic, while infected women were more likely kind-hearted, moral, diligent, conscientious, and open-minded[16].
The prevalence of toxoplasmosis in Saudi Arabia is lower than the global average, with significant variations across different age groups, water sources, and dietary habits[17]. Globally, the disease status varies from one region to another due to various reasons. The seroprevalence in Southern European countries, Southeast Asian countries, Sub-Saharan countries, and Saudi Arabia reached up to 54 %, 92.5 %, 70 %, 38 % respectively[18-21]. The prevalence rate among pregnant women in Makkah reached 35.6 %[22].
The relationship between latent toxoplasmosis and traffic accidents has been studied in many regions around the world. The first reported study was conducted in the Czech Republic in 2002, where authors found a significant relationship between traffic accidents and latent toxoplasmosis. In addition, they found that the relative risk decreased according to the duration of infection, suggesting that latent toxoplasmosis poses a very serious public health problem as well as an economic one[5]. In 2009, a study conducted in Prague confirmed that T. gondii infection has a strong impact on traffic accidents[12]. Another study conducted in Istanbul found a strong relationship between latent toxoplasmosis and traffic accidents, especially in men aged 31 y-44 y[13]. In Mexico, a study also found a link between latent toxoplasmosis and road traffic accidents but did not find any link between ocular toxoplasmosis and road traffic accidents[4].
In Saudi Arabia, the latest official annual report revealed that around 300 000 traffic accidents occurred in 2019[23].
The main aim of the current study is to evaluate the relationship between latent toxoplasmosis and traffic accidents in Al-Madinah, Saudi Arabia.
Materials and Methods
Study design and population: The present casecontrol study was conducted at King Fahad Hospital in Al-Madinah during August and November 2022. No exclusion criteria were chosen for examination in terms of age and occupation.
The study population was divided into experimental and control groups. The experimental group consisted of male drivers who were involved in traffic accidents and were referred to the emergency department of King Fahad Hospital in Al-Madinah due to injuries sustained in a recent traffic accident. The control group included randomly selected male drivers who had never been involved in traffic accidents.
Data collection:
A face-to-face interview was conducted with each participant filling out a questionnaire related to the demographic data information and the possible risk factors of infection by T. gondii. In addition to variables related to awareness about the parasite.
Blood sample collection:
A total of 86 blood samples were collected from both the experimental and control groups equally between August and November 2022. Approximately 5 ml of blood was collected from each participant in a plain vacutainer tube, then the serum was kept in cryotube after centrifugation of the blood at 5000 rpm for 10 min and then stored at -20° until use.
Serological tests:
The two-step ARCHITECT Toxo Immunoglobulin G (IgG) and Immunoglobulin M (IgM) assay was used to quantify antibodies against T. gondii infection in human serum and plasma based on Chemiluminescent Microparticle Immunoassay (CMIA) according to the manufacturer’s instructions. (Abbott GmbH, Max- Planck-Ring 265205 Wiesbaden, Germany).
Statistical analysis:
Statistical analysis was performed using Statistical Package for the Social Sciences (SPSS) version 26. Demographic data and variables were inserted. A p<0.05 considered significant. Chi-square (χ2) was used to compare frequencies between groups.
Results and Discussion
The prevalence of chronic toxoplasmosis (IgG) in the current study was 23.8 % in the drivers with a traffic accident history, while it was 0 % in control group drivers with no traffic accident history. The results obtained in the present study may associate traffic accident with chronic Toxoplasma infection (p<0.009) as shown in Table 1.
| Drivers’ status (N) | IgG | χ2 | p-value | |
|---|---|---|---|---|
| Positive (n, %) | Negative (n, %) | |||
| With traffic accidents (42) | (10, 23.8) | (32, 76.2) | 6.735 | 0.009 |
| Without traffic accidents (control) (24) | (0, 0) | (24, 100) | ||
| Total (66) | (10, 15.2) | (56, 84.8) | ||
Table 1: Chronic Toxoplasmosis Associated with Traffic Accident
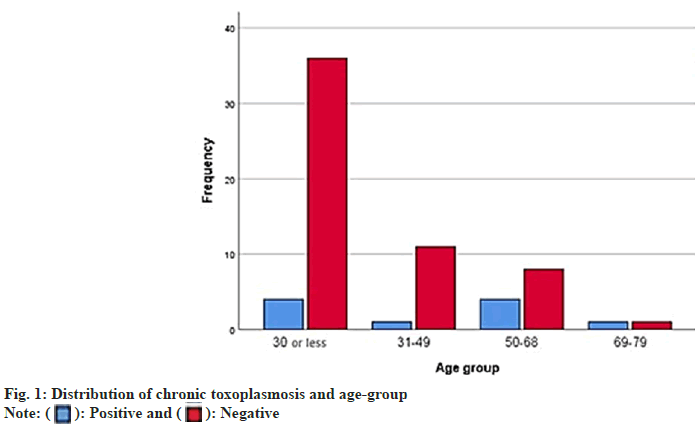
Although the results obtained from the current study show no significant correlation between chronic toxoplasmosis and age group (p>0.05), fig. 1 shows that the results were higher in the age groups less than 30 and 50 y-68 y old.
The results showed that cutting raw meat without wearing gloves may be the main source of chronic toxoplasmosis infection as shown in Table 2, (p<0.05). In addition, there was a significant difference between occupation and acquired chronic toxoplasmosis as shown in Table 2, and the retired people were more susceptible to infection compared with other groups (p<0.05).
| Factor (N) | Traffic accident | χ2 | p-value | |
|---|---|---|---|---|
| Yes (n, %) | No (n, %) | |||
| Occupation | ||||
| Student (35) | (1, 2.9) | (34, 97.1) | 11.692 | 0.02* |
| Governmental employee (10) | (2, 20) | (8, 80) | ||
| Private employee (2) | (0, 0) | (2, 100) | ||
| Retired (13) | (5, 38.5) | (8, 61.5) | ||
| Unemployed (6) | (2, 33.3) | (4, 66.7) | ||
| Frequency of traffic accidents | ||||
| None (24) | (0, 0) | (24, 100) | 10.902 | 0.012* |
| 1-2 (24) | (4, 16.7) | (20, 83.3) | ||
| 3-4 (16) | (6, 37.5) | (10, 62.5) | ||
| >5 (2) | (0, 0) | (2, 100) | ||
| Disability | ||||
| Yes (8) | (3, 37.5) | (5, 62.5) | 3.537 | 0.06 |
| No (58) | (7, 12.1) | (51, 87.9) | ||
| Close contact with cat | ||||
| Yes (45) | (9, 20) | (36, 80) | 2.586 | 0.108 |
| No (21) | (1, 4.8) | (20, 95.2) | ||
| Eating raw meat | ||||
| Yes (31) | (6, 19.4) | (25, 80.6) | 0.803 | 0.37 |
| No (35) | (4, 11.4) | (31, 88.6) | ||
| Received blood transfusion | ||||
| Yes (9) | (2, 22.2) | (7, 77.8) | 0.405 | 0.524 |
| No (57) | (8, 14.0) | (49, 86.0) | ||
| Working in the garden | ||||
| Yes (38) | (8, 21.1) | (30, 78.9) | 2.426 | 0.119 |
| No (28) | (2, 7.1) | (26, 92.9) | ||
| Aware about toxoplasmosis | ||||
| Yes (14) | (0, 0) | (14, 100) | 3.137 | 0.075 |
| No (52) | (10, 19.2) | (42, 80.8) | ||
| Drinking camel milk | ||||
| Yes (49) | (8, 16.3) | (41, 83.7) | 0.204 | 0.651 |
| No (17) | (2, 11.8) | (15, 88.2) | ||
| Drinking unpasteurized milk | ||||
| Yes (25) | (3, 12.0) | (22, 88.0) | 0.116 | 0.733 |
| No (40) | (6, 15.0) | (34, 85.0) | ||
| Cutting raw meat without using gloves | ||||
| Yes (48) | (10, 20.8) | (38, 79.2) | 4.42 | 0.036* |
| No (18) | (0, 0) | 18, (100) | ||
Table 2: Explain the Risk Factors Associated with Chronic Toxoplasmosis
Regarding traffic accidents, there was a significant difference between chronic infection and recurrence of traffic accidents, especially among drivers who committed 3-4 traffic accidents (p<0.05), as shown in Table 2.
According to the World Health Organisation (WHO), traffic accidents are one of the most important problems in terms of social, economic, and human health issues, and has estimated that approximately 1.4 million people die annually due to road traffic, making it among the top ten causes of death globally[24,25]. Another 20-50 million people suffer from non-fatal road accidents, many of whom suffer disability because of their injuries[24]. According to the Saudi Ministry of Health, the overall total number of road traffic injuries and deaths during 2018-2020 were 89050 and 16159, respectively[26].
We believe that this is the first study conducted in Saudi Arabia that links chronic toxoplasmosis and traffic accidents. This case-control study included drivers who had been involved in a traffic accident and drivers who had not been involved in a traffic accident. In agreement with previous studies conducted in Mexico, Czech Republic, Turkey, Poland, Russia, Iraq and Egypt, our results showed significant association between traffic accidents and chronic toxoplasmosis[4,5,7,12,13,27-32]. On the other hand, a very weak association between traffic accidents and toxoplasmosis was found in a recent study in Denmark[33], while no significant association was reported in a study in Jordan that included only 13 participants[34].
Flegr et al.[5], believe that the effect of latent toxoplasmosis, rather than the transient effect of acute toxoplasmosis, appears to be the most likely candidate to explain the increased risk of traffic accidents in people infected with Toxoplasma.
The current study revealed that chronic infection is related to occupation, especially retirees. This result is logical and consistent with the fact that chronic toxoplasmosis requires a long time and long follow-up.
Some biological mechanisms may explain how latent toxoplasmosis may increase the risk of traffic accidents. Elevated dopamine levels have been linked to toxoplasmosis in humans, animal models, and in vitro[35-42]. The Toxoplasma genome in infected tissues is responsible for the expression of a dopamine synthesis enzyme known as tyrosine hydroxylase[39,40,43].
Elevated dopamine concentrations have been observed in individuals with neuropsychiatric disorders, and in subjects with behavioural changes such as prolonged response time, decreased cognition and decline of long-term concentration[35,39,44]. Latent toxoplasmosis results in the production of the rate-limiting enzyme, Indoleamine-2, 3-Dioxygenase (IDO)[41,45]. This results in decreased tryptophan production, which is essential for Toxoplasma growth and replication, and furthermore leads to the secretion of harmful Kynurenic Acid (KYNA) and Quinolinic Acid (QUIN) [46]. Increased levels of KYNA and QUIN have been found in individuals with schizophrenia and have been linked to suicidal behaviours[39,47-49]. Hence, the dopamine and glutamate systems are disrupted by T. gondii, and this may involve intermediate factors between toxoplasmosis and psychiatric disorders.
Our study confirmed that drivers in Al-Madinah, Saudi Arabia who were frequently involved in traffic accidents had a significantly higher association with chronic toxoplasmosis compared to other groups[50].
We found that the source of getting toxoplasmosis among our experimental group may be due to cutting raw meat without using gloves, due to bradyzoite found in muscle tissues. At the same time, such a conclusion should not rule out the existence of cultural conditions and customs prevailing among those drivers involved in traffic accidents[51].
The results of this study support the findings of previous studies in several countries that drivers with chronic toxoplasmosis were significantly associated with traffic accidents compared to uninfected drivers. Therefore, to greatly avoid the problem of public health and economic underestimation, we recommend toxoplasmosis testing as a requirement before issuing a driver’s licence, which may play a vital role in the epidemiology of traffic accidents in Saudi Arabia.
Ethical approval:
This study was approved by the ethical committee at the Saudi Ministry of Health, (IRB013-2022). The aim and the procedures of the study were clarified to each participant and a written informed consent form was signed before enrolment in the study.
Conflict of interests:
The authors declared no conflict of interests.
References
- Khairullah AR, Kurniawan SC, Widodo A, Effendi MH, Hasib A, Silaen OS, et al. A comprehensive review of toxoplasmosis: Serious threat to human health. Open Public Health J 2024;17(1):e18749445281387.
- Atif I, Touloun O, Boussaa S. Toxoplasma gondii in humans, animals and in the environment in Morocco: A literature review. Gut Pathogens 2024;16(1):53.
[Crossref] [Google Scholar] [PubMed]
- Colzato L, Zhang W, Beste C, Stock AK. Dissociating direct and indirect effects: A theoretical framework of how latent toxoplasmosis affects cognitive profile across the lifespan. Neurobiol Aging 2021;102:119-28.
[Crossref] [Google Scholar] [PubMed]
- Galván-Ramírez MD, Sánchez-Orozco LV, Rodríguez LR, Rodríguez S, Roig-Melo E, Troyo Sanromán R, et al. Seroepidemiology of Toxoplasma gondii infection in drivers involved in road traffic accidents in the metropolitan area of Guadalajara, Jalisco, Mexico. Parasites Vectors 2013;6(1):1-294.
[Crossref] [Google Scholar] [PubMed]
- Flegr J, Havlícek J, Kodym P, Malý M, Smahel Z. Increased risk of traffic accidents in subjects with latent toxoplasmosis: A retrospective case-control study. BMC Infect Dis 2002;2:1-6.
[Crossref] [Google Scholar] [PubMed]
- Novotná M, Hanusova J, Klose J, Preiss M, Havlicek J, Roubalová K, et al. Probable neuroimmunological link between Toxoplasma and cytomegalovirus infections and personality changes in the human host. BMC Infect Dis 2005;5:1-0.
[Crossref] [Google Scholar] [PubMed]
- Yereli K, Balcio?lu IC, Özbilgin A. Is Toxoplasma gondii a potential risk for traffic accidents in Turkey? Forensic Sci Int 2006;163(1-2):34-7.
[Crossref] [Google Scholar] [PubMed]
- Ka?ková S, Kodym P, Frynta D, Vav?inová R, Kub?na A, Flegr J. Influence of latent toxoplasmosis on the secondary sex ratio in mice. Parasitology 2007;134(12):1709-17.
[Crossref] [Google Scholar] [PubMed]
- Ka?ková Š, Šulc J, Nouzová K, Fajfrlík K, Frynta D, Flegr J. Women infected with parasite Toxoplasma have more sons. Naturwissenschaften 2007;94(2):122-7.
[Crossref] [Google Scholar] [PubMed]
- Torrey EF, Bartko JJ, Lun ZR, Yolken RH. Antibodies to Toxoplasma gondii in patients with schizophrenia: A meta-analysis. Schizophr Bull 2007;33(3):729-36.
[Crossref] [Google Scholar] [PubMed]
- Arling TA, Yolken RH, Lapidus M, Langenberg P, Dickerson FB, Zimmerman SA, et al. Toxoplasma gondii antibody titers and history of suicide attempts in patients with recurrent mood disorders. J Nerv Mental Dis 2009;197(12):905-8.
[Crossref] [Google Scholar] [PubMed]
- Flegr J, Klose J, Novotná M, Berenreitterová M, Havlí?ek J. Increased incidence of traffic accidents in Toxoplasma-infected military drivers and protective effect RhD molecule revealed by a large-scale prospective cohort study. BMC Infect Dis 2009;9:1-72.
[Crossref] [Google Scholar] [PubMed]
- Kocazeybek B, Oner YA, Turksoy R, Babur C, Cakan H, Sahip N, et al. Higher prevalence of toxoplasmosis in victims of traffic accidents suggest increased risk of traffic accident in Toxoplasma-infected inhabitants of Istanbul and its suburbs. Forensic Sci Int 2009;187(1-3):103-8.
[Crossref] [Google Scholar] [PubMed]
- Miman O, Kusbeci OY, Aktepe OC, Cetinkaya Z. The probable relation between Toxoplasma gondii and Parkinson's disease. Neurosci Lett 2010;475(3):129-31.
[Crossref] [Google Scholar] [PubMed]
- Alvarado-Esquivel C, Méndez-Hernández EM, Salas-Pacheco JM, Ruano-Calderón LÁ, Hernández-Tinoco J, Arias-Carrión O, et al. Toxoplasma gondii exposure and Parkinson's disease: A case-control study. BMJ Open 2017;7(2):e013019.
[Crossref] [Google Scholar] [PubMed]
- Flegr J. Effects of Toxoplasma on human behaviour. Schizophrenia Bull 2007;33(3):757-60.
[Crossref] [Google Scholar] [PubMed]
- Cook AJ, Holliman R, Gilbert RE, Buffolano W, Zufferey J, Petersen E, et al. Sources of Toxoplasma infection in pregnant women: European multicentre case-control study commentary: Congenital toxoplasmosis-further thought for food. BMJ 2000;321(7254):142-7.
[Crossref] [Google Scholar] [PubMed]
- Moafa HN, Altemani AH, Alaklabi A, Ghailan KY, Alshabi A, Darraj MA, et al. The prevalence of Toxoplasma gondii in Saudi Arabia (1994–2023): A systematic review and meta-analysis. J Epidemiol Global Health 2024;14(4):1413-52.
[Crossref] [Google Scholar] [PubMed]
- Nissapatorn V. Toxoplasmosis: A silent threat in Southeast Asia. Res J Parasitol 2007;2(1):1-12.
- Ayi I, Edu S, Apea-Kubi KA, Boamah D, Bosompem KM, Edoh D. Sero-epidemiology of toxoplasmosis amongst pregnant women in the greater Accra region of Ghana. Ghana Med J 2009;43(3):107-14.
[Crossref] [Google Scholar] [PubMed]
- Almogren A. Antenatal screening for Toxoplasma gondii infection at a tertiary care hospital in Riyadh, Saudi Arabia. Annal Saudi Med 2011;31(6):569-72.
[Crossref] [Google Scholar] [PubMed]
- Al-Harthi SA, Jamjoom MB, Ghazi HO. Seroprevalence of Toxoplasma gondii among pregnant women in Makkah, Saudi Arabia. Umm Al-Qura Univ J Sci Med Eng 2006;18(2):217-27.
- STATS: General authority for statistics, traffic accidents location by region; 2019.
- WHO: Road traffic injuries; 2022.
- WHO: Global status report on road safety; 2018.
- SMOH: Road traffic injuries and deaths, Saudi Ministry of Health; 2021.
- Samoj?owicz D, Borowska-Solonynko A, Go?ab E. Prevalence of Toxoplasma gondii parasite infection among people who died due to sudden death in the capital city of Warsaw and its vicinity. Przegl Epidemiol 2013;67(1):29-33.
[Google Scholar] [PubMed]
- Alvarado-Esquivel C, Pacheco-Vega SJ, Hernández-Tinoco J, Salcedo-Jáquez M, Sánchez-Anguiano LF, Berumen-Segovia LO, et al. Toxoplasma gondii infection in interstate truck drivers: A case–control seroprevalence study. Parasites Vectors 2015;8:1-6.
[Crossref] [Google Scholar] [PubMed]
- Stepanova EV, Kondrashin AV, Sergiev VP, Morozova LF, Turbabina NA, Maksimova MS, et al. Significance of chronic toxoplasmosis in epidemiology of road traffic accidents in Russian Federation. PLoS One 2017;12(9):e0184930.
[Crossref] [Google Scholar] [PubMed]
- Samoj?owicz D, Twarowska-Ma?czy?ska J, Borowska-Solonynko A, Poniatowski ?A, Sharma N, Olczak M. Presence of Toxoplasma gondii infection in brain as a potential cause of risky behavior: A report of 102 autopsy cases. Eur J Clin Microbiol Infect Dis 2019;38(2):305-17.
[Crossref] [Google Scholar] [PubMed]
- Ahmed DN, Mushin S, Mohsin MA. Seroepidemiology of Toxoplasma gondii infection in drivers involved in road traffic accidents in Baghdad city. Med Legal Update 2020;20(1):814-19.
[Crossref] [Google Scholar] [PubMed]
- Hassan ZR, Zekry KM, Heikal EA, Ibrahim HF, Khirala SK, Abd El-Hamid SM, et al. Toxoplasmosis and cytomegalovirus infection and their role in Egyptian autistic children. Parasitol Res 2023;122(5):1177-87.
- Burgdorf KS, Trabjerg BB, Pedersen MG, Nissen J, Banasik K, Pedersen OB, et al. Large-scale study of Toxoplasma and Cytomegalovirus shows an association between infection and serious psychiatric disorders. Brain Behav Immun 2019:79:152-8.
[Crossref] [Google Scholar] [PubMed]
- Shotar A, Alzyoud SA, AlKhatib AJ. Latent toxoplasmosis and the involvement in road traffic accidents among a sample of Jordanian drivers. Res J Med Sci 2016;10:194-8.
- Flegr J, Preiss M, Klose J, Havl???ek J, Vitáková M, Kodym P. Decreased level of psychobiological factor novelty seeking and lower intelligence in men latently infected with the protozoan parasite Toxoplasma gondii dopamine, a missing link between schizophrenia and toxoplasmosis? Biol Psychol 2003;63(3):253-68.
[Crossref] [Google Scholar] [PubMed]
- Torrey EF, Yolken RH. Toxoplasma gondii and schizophrenia. Emerg Infect Dis 2003;9(11):1375.
- Skallová A, Novotná M, Kolbeková P, Gasova Z, Vesely V, Sechovska M, et al. Decreased level of novelty seeking in blood donors infected with Toxoplasma. Neur Lett 2005;26(5):480-6.
[Google Scholar] [PubMed]
- Skallová A, Kodym P, Frynta D, Flegr J. The role of dopamine in Toxoplasma-induced behavioural alterations in mice: An ethological and ethopharmacological study. Parasitology 2006;133(5):525-35.
[Crossref] [Google Scholar] [PubMed]
- Henriquez SA, Brett R, Alexander J, Pratt J, Roberts CW. Neuropsychiatric disease and Toxoplasma gondii infection. Neuroimmunomodulation 2009;16(2):122-33.
[Crossref] [Google Scholar] [PubMed]
- Prandovszky E, Gaskell E, Martin H, Dubey JP, Webster JP, McConkey GA. The neurotropic parasite Toxoplasma gondii increases dopamine metabolism. PloS One 2011;6(9):e23866.
[Crossref] [Google Scholar] [PubMed]
- McConkey GA, Martin HL, Bristow GC, Webster JP. Toxoplasma gondii infection and behaviour–location, location, location? J Exp Biol 2013;216(1):113-9.
[Crossref] [Google Scholar] [PubMed]
- Martin HL, Alsaady I, Howell G, Prandovszky E, Peers C, Robinson P, et al. Effect of parasitic infection on dopamine biosynthesis in dopaminergic cells. Neuroscience 2015;306:50-62.
[Crossref] [Google Scholar] [PubMed]
- Gaskell EA, Smith JE, Pinney JW, Westhead DR, McConkey GA. A unique dual activity amino acid hydroxylase in Toxoplasma gondii. PloS One 2009;4(3):e4801.
[Crossref] [Google Scholar] [PubMed]
- Eyles D, Feldon J, Meyer U. Schizophrenia: Do all roads lead to dopamine or is this where they start? Evidence from two epidemiologically informed developmental rodent models. Transl Psychiatry 2012;2(2):e81.
[Crossref] [Google Scholar] [PubMed]
- Campbell BM, Charych E, Lee AW, Möller T. Kynurenines in CNS disease: Regulation by inflammatory cytokines. Front Neurosci 2014;8:12.
[Crossref] [Google Scholar] [PubMed]
- Miller CM, Boulter NR, Ikin RJ, Smith NC. The immunobiology of the innate response to Toxoplasma gondii. Int J Parasitol 2009;39(1):23-39.
[Crossref] [Google Scholar] [PubMed]
- Sublette ME, Galfalvy HC, Fuchs D, Lapidus M, Grunebaum MF, Oquendo MA, et al. Plasma kynurenine levels are elevated in suicide attempters with major depressive disorder. Brain, behavior, and immunity. 2011;25(6):1272-8.
[Crossref] [Google Scholar] [PubMed]
- Steiner J, Bogerts B, Sarnyai Z, Walter M, Gos T, Bernstein HG, Myint AM. Bridging the gap between the immune and glutamate hypotheses of schizophrenia and major depression: Potential role of glial NMDA receptor modulators and impaired blood–brain barrier integrity. World J Biol Psychiatry 2012;13(7):482-92.
[Crossref] [Google Scholar] [PubMed]
- Erhardt S, Lim CK, Linderholm KR, Janelidze S, Lindqvist D, Samuelsson M, et al. Connecting inflammation with glutamate agonism in suicidality. Neuropsychopharmacology 2013;38(5):743-52.
[Crossref] [Google Scholar] [PubMed]
- Gohardehi S, Sharif M, Sarvi S, Moosazadeh M, Alizadeh-Navaei R, Hosseini SA, et al. The potential risk of toxoplasmosis for traffic accidents: A systematic review and meta-analysis. Exp Parasitol 2018;191:19-24.
[Crossref] [Google Scholar] [PubMed]
- Nordfjærn T, ?im?eko?lu O, Rundmo T. Culture related to road traffic safety: A comparison of eight countries using two conceptualizations of culture. Accid Anal Prev 2014;62:319-28.
[Crossref] [Google Scholar] [PubMed]
 ): Positive and (
): Positive and ( ): Negative
): Negative



