- *Corresponding Author:
- A. Sathish
Department of Clinical Pharmacy, A.R College of Pharmacy, Vallabh Vidya Nagar, Anand-388 120, India
E-mail: asathish1981@yahoo.co.in
| Date of Submission | 21 June 2010 |
| Date of Revision | 1 October 2011 |
| Date of Acceptance | 15 October 2011 |
| Indian J Pharm Sci, 2011, 73 (5): 590-592 |
Abstract
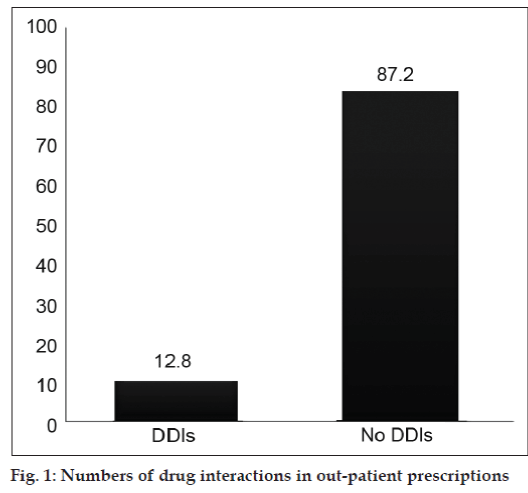
The objective of the research work was to analysis the out patients drug interactions and alerts the healthcare professionals to prevent the future complications. The study was done in three pharmacies within a 200 meters distance of each other. The doctors involved were made aware of the study but data were collected without their knowledge. All prescriptions presented to the three pharmacies were analyzed during the five-month study period. A total of 500 prescriptions were analyzed and 64 drug-drug interactions were detected giving a drug-drug interaction rate of 12.8 percent but 436 (87.2%) prescriptions are free from drug interactions. Moderate drug interactions were found in 10.2%, Severe were 2.6% and contraindicated were 0% and also disease wise drug interaction analysis were carried out during the study results, more number of drug interactions reported in central nerves system followed by diabetes mellitus. Outpatient visits resulted in minimal numbers of clinically important drug-drug interactions, these interactions can have significant implications due to medication-related morbidity and mortality. Pharmacists can play a critical role in managing the medication therapy of patients at risk for clinically important drug-drug interactions.
Keywords
Drug-drug interaction, out-patient, pharmacies, prescriptions
Drug-drug interactions (DDIs) are a concern for patients and providers, as multiple medication use is becoming more common to manage complex diseases. The consequences of DDIs can range from no untoward effects to drug-related morbidity and mortality. Although DDIs are considered preventable medication-related problems [1,2]. Research has also shown that DDIs are associated with increased health care use [3,4].
A drug-drug interaction represents a specific type of adverse drug reaction, and the risk of druginteractions is proportional to the number of drugs taken. However, although potential drug-drug interactions may affect 40-65% of all hospitalized patients, the clinical consequences of these drug interactions are highly variable, and adverse effect rarely occur [5].
The significance and appropriate management of DDIs is a continuously evolving issue for providers. Research using prescription databases can contribute to greater understanding of clinically important potential DDIs; however, only a few studies have examined clinically important DDIs in the outpatient setting, and even fewer studies have identified patients at risk for such DDIs [6-10]. Despite outpatients receiving drug pairs with a high potential for adverse interactions, the rate of occurrence of clinical drug interaction events was low [11]. The relative importance of drug interactions as a clinical problem remains unclear. Screening programs that do more than simply identify large numbers of patients who receive potentially interacting drug combinations without indicating which subpopulations of these individuals are likely to be harmed by the drugs have not yet been developed [12].
The study was done in three pharmacies within a 200 meter distance of each other. The doctors were from general practices located near these pharmacies. The doctors involved were made aware of the study but data were collected without their knowledge. All 500 prescriptions are collected during the five-month study period.
A pilot study was done in the three community pharmacies to analyze the DDIs in out-patient prescriptions. Required numbers of prescriptions were collected from the community pharmacist based pharmacy with the permission of pharmacy directors and patients. Objective of the study was explained to the patients for collecting the prescriptions. Prescriptions are collected alternatively for the combinations of mixed data’s during the study period.
All collected prescriptions from the three pharmacies were analyzed during the study period. The collected prescriptions from three pharmacies were thoroughly assessed for the presence of drug interactions. The assessments of drug-drug interactions were mainly done with the help of various tools like Medscape drug interaction online checker, books and journals. This study has demonstrated a wide range of DDIs of out-patient prescriptions from general practice, used as well as already dispensed prescriptions. A total of 500 prescriptions were taken up and required information were collected (Table 1). The collected information was analyzed. This study was concluded as follows. Out of 500 prescriptions, 64 (12.80%) prescriptions containing drug-drug interactions but 436 (87.2%) prescriptions are free from drug interactions. Moderate drug interactions were found in 51 (10.20%), Severe were 13 (2.60%) and contraindicated were 0% (Table 2). Major number of drug interactions was found in moderate drug interactions only. An attempt was made to analyze the number of prescription according to their disease found in drug interactions. The study shows that major numbers of prescriptions with drug interactions were found in central nerves system 38.46% (5) of prescription having drug interactions out of 13 prescriptions, followed by diabetes mellitus 23.63% (13) out of 55 prescriptions, respiratory system 15.88% (17) out of 107 prescriptions, cardio vascular system 13.84% (9) out of 65 prescriptions, skin reactions 8.33% (1) out of 12 prescriptions, gastro intestinal tract system 7.86% (7) out of 89 prescriptions, fever/pain 7.08% (9) out of 127 prescriptions and other prescriptions 14.28% (3) out of 21 prescriptions, more over arthritis and tuberculosis diseases prescriptions shows 0% interactions (Table 3).
| Prescriptions | Number | Percentage (%) |
|---|---|---|
| Prescriptions with drug interactions | 64 | 12.8 |
| Prescriptions without drug | 436 | 87.2 |
| interactions |
The overall analysis of total prescription (500) shows that 12.8% having drug interactions and 87.2% having no drug interaction.
Table 1: Data Showing Number Of Prescription With Drug Interactions
| Type of drug interaction | Total | Percentage (%) |
|---|---|---|
| Moderate | 51 | 10.2 |
| Severe | 13 | 2.6 |
| Contraindicated | 00 | 00 |
Out of 500 prescriptions, the Moderate drug interactions were 10.2%, severe were 2.6% and contraindication were 0%. The major types were Moderate type of drug interactions.
Table 2: Data showing types of drug interactions
| Disease | Total no. of prescriptions | Total no. of drug interactions | Percentage (%) |
|---|---|---|---|
| Fever/Pain | 127 | 9 | 7.08 |
| Respiratory system | 107 | 17 | 15.88 |
| Cardio vascular system | 65 | 9 | 13.84 |
| Gastro intestinal tract | 89 | 7 | 7.86 |
| system | 55 | 13 | 23.63 |
| Diabetes mellitus | 8 | 00 | 00 |
| Arthritis | 12 | 1 | 8.33 |
| Skin reactions | 3 | 00 | 00 |
| Tuberculosis | 13 | 5 | 38.46 |
| Central nerves system | 21 | 3 | 14.28 |
| Others total | 500 | 64 | ---- |
This study shows that major numbers of prescriptions with drug interactions were found in central nerves system 38.46%, followed by diabetes mellitus 23.63%, respiratory system 15.88%, cardio vascular system 13.84%, skin reactions 8.33%, gastro intestinal tract system 7.86%, fever/pain 7.08% and other prescriptions 14.28%.
Table 3: Data showing number of drug interaction prescriptions in each disease
In addition, with the patient’s permission, the pharmacist may call the physician to get essential information about the prescriptions to rectify the drug interactions apart from educating healthcare professionals about the importance of drug interactions because outpatient prescriptions contains very minimal amount of drug interactions in that 10.20% prescriptions are moderate drug interactions as well as preventable and only 2.60% of severe interactions were detected, the amount of outpatients prescription drug interactions are very low.
Out-patient based prescriptions are contains few drugs and the analysis shown very little amount of drug interactions (fig. 1) but patients are also purchasing the medications without prescriptions and consultations with the healthcare professionals, it may lead to drug related problems and produce adverse events. Many drug interactions can be avoided or managed safely from the pharmacist side by assessing possible drug interaction in case of multiple therapies, providing patient counseling on the use of prescription and nonprescription medication, disease state(s) and the safety of concurrent use of herbal products. Preventing and/or managing drug interactions will be more likely to occur when the pharmacist takes time and utilizes and adequate patient data base.
Acknowledgements
Authors are thankful to all the doctors of the hospital, out patient’s clinical practice, pharmacy directors, and pharmacy in-chargers to carry out this study.References
- Juurlink DN, Mamdani M, Kopp A, Laupacis A. Drug-drug interactions among elderly patients hospitalized for drug toxicity. JAMA 2003;289:1652-8.
- McDonnell PJ, Jacobs MR. Hospital admissions resulting from preventable adverse drug reactions. Ann Pharmacother 2002;3 6:1331-6.
- Hamilton RA, Briceland LL, Andritz MH. Frequency of hospitalization after exposure to known drug-drug interactions in a Medicaid population. Pharmacotherapy 1998;18:1112-20.
- Jankel CA, McMillan JA, Martin BC. Effect of drug interactions on outcomes of patients receiving warfarin or theophylline. Am J Hosp Pharm 1994;51:661-6.
- Glintborg B, Andrersan SE, Dalhoff K. Drug-Drug interactions among recently hospitalized patients-frequent but mostly clinically insignificant. Eur J ClinPharmacol 2005;61:675-81.
- Zhan C, Correa-de-Araujo R, Bierman AS, Sangl J. Suboptimal prescribing in elderly outpatients: Potentially harmful drug-drug and drug-disease combinations. J Am GeriatrSoc 2005;53:262-7.
- Solberg LI, Hurley JS, Roberts MH. Measuring patient safety in ambulatory care: Potential for identifying medical group drug-drug interaction rates using claims data. Am J Manag Care 2004; 10:753-9.
- Peng CC, Glassman PA, Marks IR, Fowler C, Castiglione B, Good CB. Retrospective drug utilization review: Incidence of clinically relevant potential drug-drug interactions in a large ambulatory population. J Manag Care Pharm 2003;9:513-22.
- Malone DC, Hutchins DS, Haupert H. Assessment of potential drug-drug interactions with a prescription claims database. Am J Health Syst Pharm 2005;62:1983-91.
- Lafata JE, Schultz L, Simpkins J. Potential drug-drug interactions in the outpatient setting. Med Care 2006;44:534-41.
- Janchawee B, Owatranporn T, Mahatthanatrakul W, Chongsuvivatwong V. Clinical drug interactions in outpatients of a university hospital in Thailand. J Clin Pharm Ther 2005;30:583-90.
- Jankel CA, Speedie SM. Detecting drug interactions: A review of the literature. DICP 1990;24:982-9.