- *Corresponding Author:
- R. Lin
Departments of Neurosurgery, Zhangzhou Affiliated Hospital of Fujian Medical University, Zhangzhou, Fujian 363000, China
E-mail: linruisheng0189@126.com
|
This article was originally published in Special issue, “Trends in Therapeutic Management of Various Clinical Conditions-II” |
| Indian J Pharm Sci 2021:83(2)Spl issue8;7-11 |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
The safety and clinical efficacy of superficial temporal artery-middle cerebral artery bypass grafting combined with superficial temporal artery branching and cerebral-dural-temporal vascular grafting in the treatment of adult moyamoya disease are investigated. A retrospective analysis of the data of 22 adult patients with moyamoya disease who underwent superficial temporal artery-brain artery bypass grafting combined with superficial temporal artery branching and cerebral-dural-muscle vascular stenting from June 2012 to June 2018 is performed to analyze the patient’s treatment outcome, functional recovery, and complications. Among the 22 patients, 17 (77.3 %) patients have improved clinical symptoms 1 w after surgery, and 5 patients (22.7 %) have no significant improvement in symptoms. After 3 mo follow-up, 21 patients (95.5 %) have significant improvement in clinical symptoms and spontaneous living ability compared with preoperative, and 1 patient (5.3 %) has no improvement in symptoms of new cerebral infarction. In patients with ischemic moyamoya disease, the clinical symptoms and quality of life of patients with superficial temporal artery-middle cerebral artery bypass graft combined with superficial temporal artery branching and cerebral-dural-temporal muscle vascularization are significantly improved. It shows that it can improve the prognosis of patients with ischemic moyamoya disease and has important clinical significance for the recovery of neurological function and the improvement of quality of life.
Keywords
Moyamoya disease, superficial temporal artery-brain middle artery bypass, superficial temporal artery branching, diaphragmatic vascular grafting
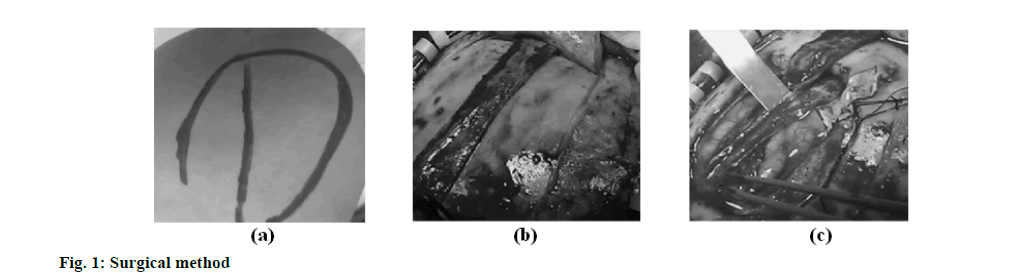
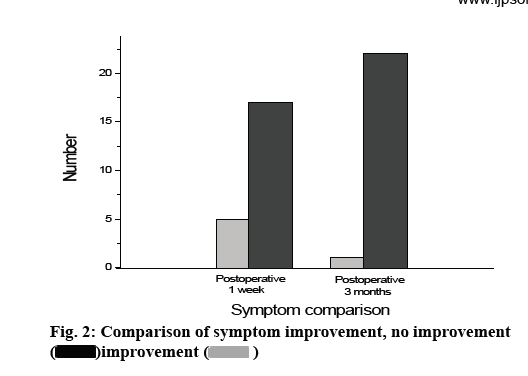
Moyamoya disease is a rare cerebrovascular disease. Its characteristic pathological manifestation is the progressive stenosis of the end of the internal carotid artery, causing a progressive decline in cerebral blood flow, and a large amount of abnormal hyperplasia pathologically compensated from the skull base. The vascular network forms a collateral circulation. The final outcome of moyamoya disease is complete occlusion of the internal carotid artery, which is ultimately provided by the external carotid artery system or the vertebral artery system[1-3]. Current epidemiological studies on moyamoya disease show that the incidence of moyamoya disease is about 10/10 million, and the incidence of men is lower than that of women, which is about 1:1.8. The clinical manifestations of moyamoya disease are mainly divided into ischemic and hemorrhagic types. Among them, adult ischemic moyamoya disease mainly includes Transient Ischemic Attack (TIA), paresthesia, epilepsy, mental retardation, dyskinesia, etc. Some patients may have no obvious clinical symptoms. A saccular aneurysm or abnormally smog-like vascular rupture in the Willis ring is the leading cause of intracranial hemorrhage. Vascular-like vascular rupture often occurs in the basal ganglia and thalamus and often breaks into the lateral ventricle and the third ventricle. Long-term hemodynamic stress causes vascular pathological changes is an important cause. At present, the clinical treatments for ischemic moyamoya disease include surgical treatment and medical treatment. The ultimate goal is to ensure the maximum supply of cerebral blood flow, ensure the quality of life of patients, and prevent the occurrence of acute stroke events. Surgical treatment mainly involves revascularization, including direct bypass, indirect bypass and combined bypass. It can increase cerebral blood perfusion and establish effective collateral circulation to improve the clinical symptoms and quality of life of patients[4]. Among them, direct revascularization can rapidly improve cerebral blood perfusion in patients, but it requires higher micromanipulation techniques. Direct blood supply reconstruction includes: superficial temporal arterymiddle cerebral artery (STA-MCA) anastomosis, superficial temporal artery-anterior cerebral artery (STA-ACA) anastomosis, superficial temporal arteryposterior cerebral artery (STA-PCA) anastomosis and occipital artery-posterior cerebral artery (OA-PCA) anastomosis. A variety of direct blood supply reconstruction can immediately establish collateral circulation. The specific surgical method depends on the blood supply reconstruction area and the corresponding vascular condition (donor, recipient arterial diameter and distance, with or without collateral circulation, etc.). STA-MCA anastomosis is the most common. There are many types of indirect blood supply reconstruction, including: brain-muscle muscle application (encephalo-myo-synangiosis (EMS)), brain-arterial application (encephalo-arteriosynangiosis (EAS)), brain-dural placement (encephaloduro- synangiosis (EDS)), brain-cap deciduamusculoskeletal application (encephalo-galeo-myosynangiosis (EGMS)), cerebral-cap decidual smear (encephalo-galeo synangiosis (EGS)), cerebral-duralarterial vascular fusion (Encephalo-duro-arteriosynangiosis (EDAS)), cerebral-dural-arterial-muscle musculature (encephalo-duroarterio-myo-synangiosis (EDAMS)), cerebral-dural-arterial-diaphragmperiosteal appendage (encephalo-duro-myo-arteriopericranio- synangiosis (EDMAPS)), multiple intracranial drilling (Multiple burr hole (MBH)), brainmajor ointment (end of study-EOS), periarterial sympathectomy and Cervical ganglionectomy, etc.[5-7]. At present, EAS, EDS, carotid sympathectomy and superior cervical ganglionectomy have been used less frequently because of their poorer efficacy than subsequent surgical procedures. EOS requires a traumatic abdominal surgery and is currently only used for refractory moyamoya disease with poor blood supply for the first time. EMS is first used by Karasawa to treat moyamoya disease and is the earliest indirect procedure for moyamoya disease[8-10]. Retrospective analysis of 22 adult patients with moyamoya disease who underwent superficial temporal artery-brain artery bypass grafting combined with superficial temporal artery branching and cerebral-dural-muscle vascular stenting from June 2012 to June 2018 is carried out. There are 12 males and 10 females. The age is from 25 to 66 y old, and the average age is 35.5±19.3 y old. There are 3 cases on one side and 19 cases on both sides. 5 cases of hemorrhage type, 6 cases of infarction type, 6 cases of TIA type, 3 cases of frequent TIA type (the number of attacks is greater than twice a month), and 2 cases of epilepsy type. There are 5 cases in stage II of Suzuki, 10 cases in stage III, 4 cases in stage IV, and 3 cases in stage V. Suzuki stage II is staged in 5 cases, stage III in 10 cases, stage IV in 4 cases, and stage V in 3 cases. Twenty two patients with moyamoya disease undergo 27 lateral hemisphere operations. The informed consent signed by the patients or their family members was obtained and this study was approved by the medical ethics committee of Zhangzhou Affiliated Hospital of Fujian Medical University. Inclusion criteria: First, refer to Japan’s 2012 moyamoya disease diagnosis and treatment guidelines, patients who are confirmed by whole brain angiography, included in bilateral and unilateral moyamoya disease are selected. The end of the internal carotid artery or the anterior cerebral artery and/or the middle cerebral artery is narrow or occluded. In the arterial phase, abnormal cerebral vascular network occurs near the stenotic or occluded blood vessels. Second, patients with relevant clinical symptoms who agree to receive new surgical treatment are selected. Third, patients who are followed up for more than 6 mo are selected. Exclusion criteria: First, extracranial blood vessels are more compensated for intracranial blood supply, and surgery may destroy the original compensation. Second, patients in the acute phase of cerebral infarction and cerebral hemorrhage are excluded. Third, patients with frequent epileptic seizures without drug control are excluded. Fourth, patients with moyamoya disease who have underlying diseases such as atherosclerosis, hyperthyroidism, neurofibromatosis, and autoimmune diseases are excluded. Fifth, large-area cerebral infarction and other reasons can be excluded. Under general anesthesia, patients undergo surgery on the symptom side and severe ischemic side. Doppler ultrasound or finger touch is used to find the stroke of the superficial temporal artery and mark it. According to preoperative cerebral angiography, cerebral perfusion imaging and clinical symptoms, the surgical approach is to improve the pterional approach. During the operation, the anterior and posterior branches of the superficial temporal artery are carefully separated, the diaphragm and skull are separated to the level of the zygomatic arch, the bone flap is removed, the dura mater is suspended, the dura mater is cut, and the dura is re-folded and applied to the brain surface after complete hemostasis. The vascular region of the middle cerebral artery cortex branch with the diameter of the donor artery is selected to open the arachnoid membrane, temporarily block the superficial temporal artery and the middle cerebral artery branch and prepare for anastomosis. The superficial temporal artery and middle cerebral artery are washed with heparin saline. End-toside anastomosis of the superficial temporal artery and the middle cerebral artery cortex branch is performed with a vascular anastomosis line. After the anastomosis, the blockage is opened, and it is observed whether the anastomosis is exact, whether there is bleeding and whether the anastomosis is smooth. After the determination is made, the diaphragmatic muscle flap is adhered to the brain tissue and the edge of the diaphragm is sutured at the dura reflex. Part of the lower edge of the bone flap is removed and then reset. During surgery, it should be noted that the flap should be as large as possible to cover the ischemic area and reduce the risk of scalp ischemia, as shown in fig. 1a. The bone flap is designed according to the size of the fascial flap, as shown in fig. 1b, and the bone window is reserved. Multiple arachnoid membranes are dissected, as shown in fig. 1c, and the fascia flap is sutured to the edge of the dural incision. All patients enrolled are assessed for modified Rankin Score (mRS) (liability ability score) and Modified Barthel Index (MBI) (living activities ability score) for clinical symptoms and daily living ability on the day before surgery, 1 w after surgery, and 3 mo after surgery. The mRS has a total score of 6 points. The specific scoring criteria are shown in Table 1. Each activity rating in the MBI rating basic rating can be divided into 5 levels (5 points). Different levels represent different levels of independence. The higher the level is, the higher the independence is. Evaluation results: normal is 100 points; ≥60 points, life is basically self-care; 41-59 points, moderate dysfunction, life needs help; 21-40 points, severe dysfunction, life dependence is obvious; ≤20 points, life is completely dependent[11,12]. The operation is smooth, and all patients have no serious complications such as intracranial hematoma after surgery. 1 w after surgery, 17 (77.3 %) of the 22 patients have improved clinical symptoms, and 5 patients (22.7 %) have no significant improvement in symptoms. After 3 mo follow-up, 21 patients (95.5 %) have significant improvement in clinical symptoms and spontaneous living ability compared with preoperative ones. One patient (5.3 %) has no improvement in symptoms after surgery for new cerebral infarction. The lateral limb muscle strength decreases, but the clinical symptoms improve compared with 1 w after surgery, as shown in fig. 2. All patients have no bleeding or infarction of the new or contralateral cerebral hemisphere during the 3 mo follow-up period. The preoperative mRS score and MBI score are compared with Wilcoxon signed rank test for 1 w after operation, p>0.05. The results are not statistically significant. The preoperative mRS score and MBI score are compared with the postoperative 3 mo. The difference is statistically significant, p<0.05, as shown in Table 2. The results show that with the continuous effect of postoperative revascularization, the clinical symptoms and quality of life of patients are not significantly improved in the short term, which may be related to the formation of collateral circulation, intracranial reperfusion time and recovery of neurological function. From the long-term recovery, the patient’s clinical symptoms and quality of life have been significantly improved. It shows that it can improve the prognosis of patients with ischemic moyamoya disease, and has important clinical significance for the recovery of neurological function and the improvement of quality of life. There are 4 cases of complications in 22 patients, including 2 cases of cerebral infarction, 2 cases of subdural hematoma and 2 cases of scalp ischemia. Except for 1 case of hair growth disorder, no surgical related sequelae are left. In order to avoid surgical complications, attention should be paid during surgery. First, according to the angiographic results, the surgery is rationally designed to avoid the original compensation damage, avoid hypercapnia, hypotension, hypovolemia, hypohematocrit. Correcting anemia can reduce the incidence of postoperative cerebral infarction and transient symptoms. Wide flaps and flaps with 1.5 cm or more fascia on the edge of the flap can reduce scalp ischemia. It is also necessary to avoid too thin flaps leading to cerebral ischemic necrosis or hair loss. Third, when resetting the bone flap and diaphragm, the superficial temporal artery and its fascia flap must be not compressed, so as not to affect the surgical effect. Fourth, if intraoperative dura mater and arachnoid integrity are impaired, subcutaneous effusion may occur, so the flap should be tightly sutured to avoid extravasation of cerebrospinal fluid. Moyamoya disease is a chronic progressive cerebral vascular occlusive disease with the Willis ring of the brain. It is mainly unilateral or bilateral internal carotid artery distal cerebral artery and anterior cerebral artery stenosis or occlusion with cranial base and pia mater and small blood vessels. At present, the specific cause of moyamoya disease has not been clearly stated. However, through a large number of intraoperative observations and histopathological examinations, it is found that the main branches of the Willis ring in the brain of patients with moyamoya disease are characterized by thickening of the intima of the arteries, irregular thickening or thinning of the inner elastic layer, and thinning of the media. In the historical process of treating adult moyamoya disease, the treatment of intracranial and extracranial revascularization by surgery has been a controversial topic, and there is no consensus on the best treatment for adult moyamoya disease. However, it is worth noting that some patients have improved clinical symptoms after undergoing intracranial and extravascular revascularization. The combined application of direct and indirect blood supply reconstruction can improve cerebral blood supply and benefit for a long time in a short period of time, but the surgical procedure is relatively complicated and takes a long time. The combined application of multiple indirect blood supply reconstruction can expand the range of collateral reconstruction and increase the blood supply reconstruction effect. For patients with poor clinical outcomes after initial surgery and poor blood supply reconstruction, it is feasible to perform surgery again. The reoperation should be fully evaluated for its possible effects on the existing collateral circulation, as well as the arteries and vascularized tissue available for blood supply reconstruction, so that a reasonable procedure can be used to design the surgical procedure to achieve a smooth operation, reduce complications and obtain good blood supply for reconstruction purposes. Through this study, it is found that the superficial temporal artery-middle cerebral artery bypass graft combined with superficial temporal artery branching and cerebral-dural-temporal vascular stenosis can improve the therapeutic effect more effectively, which is worthy of further clinical application. However, due to the complexity of adult moyamoya disease, and the lack of sample size, short follow-up time, and lack of perfect preoperative and postoperative cerebral perfusion imaging, the results of the study have certain limitations and should be further studied through a larger number of prospective clinical case studies, so as to determine the therapeutic effect of surgery on adult moyamoya disease.
Acknowledgements:
None
Author’s contribution:
C. Xing and W. Cai equally contributed to this work.
Conflict of Interests:
The authors declared no conflict of interest.
References
- Kazumata K, Kamiyama H, Saito H, Maruichi K, Ito M, Uchino H, et al. Direct Anastomosis Using Occipital Artery for Additional Revascularization in Moyamoya Disease After Combined Superficial Temporal Artery-Middle Cerebral Artery and Indirect Bypass. Oper Neurosurg 2017;13(2):213-23.
- Aburakawa D, Fujimura M, Niizuma K, Sakata H, Endo H, Tominaga T. Navigation-guided clipping of a de novo aneurysm associated with superficial temporal artery-middle cerebral artery bypass combined with indirect pial synangiosis in a patient with moyamoya disease. Neurosurg Rev 2017;40(3):517-21.
- Kwon WK, Kwon TH, Park DH, Kim JH, Ha SK. Efficacy of superficial temporal artery-middle cerebral artery bypass in cerebrovascular steno-occlusive diseases: hemodynamics assessed by perfusion computed tomography. Asian J Neurosurg 2017;12(3):519-24.
- Suzuki H, Mikami T, Komatsu K, Noshiro S, Miyata K, Hirano T, et al. Assessment of the cortical artery using computed tomography angiography for bypass surgery in moyamoya disease. Neurosurg Rev 2017;40(2):299-307.
- Li X, Huang Z, Wu MX, Zhang D. Effect of Adventitial Dissection of Superficial Temporal Artery on the Outcome of Superficial Temporal Artery-Middle Cerebral Artery Bypass in Moyamoya Disease. Aging Dis 2017;8(4):384-91.
- Hirano T, Mikami T, Suzuki H, Hirano T, Kimura Y, Komatsu K, et al. Occipital artery to middle cerebral artery bypass in cases of unavailable superficial temporal artery. World Neurosurg 2018;112:101-8.
- Ogawa S, Ogata T, Shimada H, Abe H, Katsuta T, Fukuda K, et al. Acceleration of blood flow as an indicator of improved hemodynamics after indirect bypass surgery in Moyamoya disease. Clin Neurol Neurosurg 2017;160:92-5.
- Zhao J, Liu H, Zou Y, Zhang W, He S. Clinical and angiographic outcomes after combined direct and indirect bypass in adult patients with moyamoya disease: a retrospective study of 76 procedures. Exp Ther Med 2018;15(4):3570-6.
- Shulman JG, Snider S, Vaitkevicius H, Babikian VL, Patel NJ. Direct visualization of arterial emboli in Moyamoya syndrome. Front Neurol 2017;8:425.
- Uchino H, Kim JH, Fujima N, Kazumata K, Ito M, Nakayama N, et al. Synergistic interactions between direct and indirect bypasses in combined procedures: the significance of indirect bypasses in moyamoya disease. Neurosurgery 2017;80(2):201-9.
- Zhu F, Qian Y, Xu B, Gu Y, Karunanithi K, Zhu W, et al. Quantitative assessment of changes in hemodynamics of the internal carotid artery after bypass surgery for moyamoya disease. J Neurosurg 2017;129(3):677-83.
- Cheung AH, Lam AK, Ho WS, Tsang CP, Tsang AC, Lee R, et al. Surgical outcome for Moyamoya disease: clinical and perfusion computed tomography correlation. World Neurosurg 2017;98:81-8.
 )improvement (
)improvement ( )
)



