- *Corresponding Author:
- G. Xia
Department of Health Care, Tianjin Medical University General Hospital, Heping, Tianjin 300052, China
E-mail: tjzyylsb@163.com
| This article was originally published in a special issue, “Novel Therapeutic Approaches in Biomedicine and Pharmaceutical Sciences” |
| Indian J Pharm Sci 2021:83(6) Spl Issue “73-78” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
To investigate the risk factors of ventilator-associated pneumonia in elderly patients with acute cerebral infarction and to provide guidance for clinical prevention and treatment is the main objective. Gramnegative bacteria 38 strains (67.86 %), Gram-positive bacteria 15 strains (26.79 %) and fungi 3 strains (5.36 %) were detected by pathogenic bacteria culture. There was no significant difference in age, gender, body mass index, smoking, drinking, hypertension, diabetes and coronary heart disease between ventilator-associated pneumonia group and non-ventilator-associated pneumonia group (p>0.05); there were significant differences between ventilator-associated pneumonia group and non-ventilator-associated pneumonia group in antibiotic prophylactic use, time of ventilator use, acute physiology and chronic health evaluation II score and serum albumin level (p<0.05). The receiver operating characteristic curve was drawn and the results showed that the sensitivity of acute physiology and chronic health evaluation II score in predicting ventilator-associated pneumonia in patients with acute cerebral infarction was 93.71 %, the specificity was 77.61 % and the area under the curve value was 0.894. The sensitivity and specificity of albumin in predicting ventilator-associated pneumonia in elderly patients with acute cerebral infarction were 78.51 %, 76.92 % and 0.857 respectively. Multivariate logistic analysis showed that prophylactic use of antibiotics and high serum albumin level could effectively reduce the risk of ventilator-associated pneumonia in elderly patients with acute cerebral infarction undergoing endotracheal intubation and mechanical ventilation (p<0.05), while prolonged time of ventilator use and increased acute physiology and chronic health evaluation II score would increase the risk of ventilator-associated pneumonia in elderly patients with undergoing endotracheal intubation and mechanical ventilation (p<0.05). There are many factors influencing the occurrence of ventilator-associated pneumonia in the elderly patients with acute cerebral infarction undergoing endotracheal intubation and mechanical ventilation, and the intervention according to the risk factors has a positive preventive effect.
Keywords
Acute cerebral infarction, ventilator-associated pneumonia, mechanical ventilation, endotracheal intubation
Acute Cerebral Infarction (ACI) is a common disease in neurology. It is common in the elderly population. The clinical manifestations include dizziness, nausea, hemiplegia and speech dysfunction, which may easily lead to cerebral ischemia and further loss of neurological function [1]. Therefore, the basic principle for the treatment of patients with ACI is to protect the brain tissue of the patients. Ventilator-Associated Pneumonia (VAP) is a serious hospital-acquired pneumonia that occurs within 48 h after mechanical ventilation and within 48 h after extubation, in which pneumonia with a mechanical ventilation duration of ≤4 d is an earlyonset VAP and late-onset VAP with a mechanical ventilation duration is ≥5 d [2]. The related literatures reported that the incidence of VAP was 15 %-60 % and the mortality was as high as 76 % [3]. The study on ACI combined with VAP at home and abroad is to obtain better curative effect by different treatment methods or to analyze the research status and risk factors of VAP, but the comprehensive analysis on elderly patients with VAP is relatively rare in patients with ACI [4]. This study retrospectively analyzed 174 elderly patients with ACI undergoing endotracheal intubation and mechanical ventilation in our hospital to explore the risk factors of VAP in elderly patients with ACI so as to provide guidance for clinical prevention and treatment.
Materials and Methods
Data:
VAP retrospective analysis was made on 174 elderly patients with ACI treated with endotracheal intubation and mechanical ventilation in Intensive Care Unit (ICU) of our hospital. The patients were divided into VAP group (n=56) and non-VAP group (n=118) from January 2018 to December 2020. Inclusion criteria: ACI diagnostic criteria refer to the diagnostic criteria formulated by the 4th National Academic Conference on Cerebrovascular Diseases in 1996 [5]; VAP diagnostic criteria refer to the criteria in the Guidelines for the Diagnosis and Treatment of Pneumonia (draft) issued by the Hospital of Chinese Society of Respiratory Disease, Chinese Medical Association [6]; patients were treated with VAP for more than 48 h; pulmonary shadow infiltration and inflammatory changes were found on chest X-ray examination; subjects data were complete. Exclusion criteria: Lung tumor; patients with pulmonary fibrosis and lung abscess; autoimmune disease; patients with psychiatric disorders.
In VAP group, there were 35 males and 21 females, aged from 51 to 87 y (mean 67.3±7.6 y) and the Body Mass Index (BMI) was 22.7±2.3 kg/m2. In non-VAP group, there were 68 males and 50 females, aged 47-86 y (mean 66.4±8.1 y) and BMI 23.0±2.1 kg/m2. There was no significant difference in age, gender and BMI between the two groups (p>0.05).
Methods:
Treatment collection: The basic data of age, gender, smoking, alcohol consumption, concomitant diseases, application of antibacterial drugs, time of ventilator use, Acute Physiology and Chronic Health Evaluation (APACHE II) score and serum Albumin (ALB) in the two groups were statistically analyzed.
The etiological results of sputum specimens of patients were analyzed retrospectively. The detection method is to collect the specimen of lower respiratory tract secretion of the patient. Firstly make routine smear and macroscopical observation, when the number of neutrophils in each field is greater than 25 and the number of epithelial cells is less than 10 or the ratio of the two is greater than 2.5:1, it is regarded as qualified specimen. Inoculate the sample in culture medium, culture at 37° for 48 h and screen qualified colonies.
The instrument for strain identification is VITEK2 compact automated microbial identification system manufactured by Biomerieux Company of France. The isolated strains are treated by Kirby-Bauer (K-B) disk diffusion method or minimum inhibitory concentration method recommended by World Health Organization (WHO). Susceptibility results were determined according to the American Association for Clinical Laboratory Standards [7].
APACHE II score [8] is composed of three parts: Acute Physiology Score (APS), age and Chronic Health Score (CPS); APS deletes the 34 parameters of APACHE, such as plasma osmotic pressure, blood lactic acid concentration, Blood Urea Nitrogen (BUN), Glucose (GLU), ALB, Central Venous Pressure (CVP) and urine volume into 12 parameters (all are the worst within the first 24 h after admission to ICU), each item is still 0-4 points and the total score is 0-60 points. Age ranged from 0 to 6, CPS ranged from 2 to 5 and APACHE II ranged from 0 to 71, with higher scores indicating more severe disease.
Statistical processing:
Statistical Package for the Social Sciences (SPSS) 21.0 software was used for statistical analysis. The age, antimicrobial prophylaxis, duration of ventilator use, APACHE II score and serum ALB level were expressed by x±s and t test was used for comparison between the two groups. The gender, smoking, alcohol consumption, hypertension, diabetes and coronary heart disease were analyzed by χ2 test. Logistic regression analysis was used for multivariate analysis, p<0.05 was used for statistical significance.
Results and Discussion
Pathogenic bacteria status of 56 patients with VAP is explained here. A total of 38 strains (67.86 %) of Gramnegative bacteria, 15 strains (26.79 %) of Gram-positive bacteria and 3 strains (5.36 %) of fungi were detected by pathogenic bacteria culture (Table 1).
| Pathogenic bacteria | Number of strains | Composition ratio |
|---|---|---|
| Gram-negative bacteria | 38 | 67.86 % |
| Pseudomonas aeruginosa | 11 | 19.64 % |
| Klebsiella pneumoniae | 8 | 14.29 % |
| Acinetobacter baumannii | 7 | 12.50 % |
| Escherichia coli | 7 | 12.50 % |
| Other | 5 | 8.93 % |
| Gram-positive bacteria | 15 | 26.79 % |
| Staphylococcus aureus | 7 | 12.50 % |
| Staphylococcus epidermidis | 5 | 8.93 % |
| Streptococcus pneumoniae | 2 | 3.57 % |
| Other | 1 | 1.79 % |
| Fungal infection | 3 | 5.36 % |
Table 1: Pathogenic Bacteria Status of 56 Patients With VAP
Various parameters between VAP group and non- VAP group were compared. There was no significant difference in age, gender, BMI, smoking, alcohol consumption, hypertension, diabetes and coronary heart disease between VAP group and non-VAP group (p>0.05); there was statistically significant difference in antimicrobial prophylaxis, time of ventilator use, APACHE II score and serum ALB level between VAP group and non-VAP group (p<0.05) (Table 2).
| General data | VAP group (n=56) | Non-VAP group (n=118) | t/c2 value | p value |
|---|---|---|---|---|
| Age (y old) | 67.3±7.6 | 66.4±8.1 | 0.698 | 0.486 |
| BMI (kg/m2) | 22.7±2.3 | 23.0±2.1 | -0.854 | 0.395 |
| Gender | 0.373 | 0.541 | ||
| Male | 35 (62.5) | 68 (57.63) | ||
| Female | 21 (37.5) | 50 (42.37) | ||
| Smoking | 1.317 | 0.251 | ||
| Yes | 22 (39.29) | 36 (30.51) | ||
| No | 34 (60.71) | 82 (69.49) | ||
| Alcohol consumption | 1.583 | 0.208 | ||
| Yes | 26 (46.43) | 43 (36.44) | ||
| No | 30 (53.57) | 75 (63.56) | ||
| Hypertension | 2.344 | 0.126 | ||
| Yes | 34 (60.71) | 57 (48.31) | ||
| No | 22 (39.29) | 61 (51.69) | ||
| Diabetes | 1.587 | 0.208 | ||
| Yes | 23 (41.07) | 37 (31.36) | ||
| No | 33 (58.93) | 81 (68.64) | ||
| Coronary heart disease | 1.435 | 0.231 | ||
| Yes | 11 (19.64) | 15 (12.71) | ||
| No | 45 (80.36) | 103 (87.29) | ||
| Prophylactic use of antimicrobials | 4.909 | 0.027 | ||
| Yes | 18 (32.14) | 59 (50) | ||
| No | 38 (67.86) | 59 (50) | ||
| APACHE II score | 6.372 | 0.012 | ||
| ≥15 points | 26 (46.43) | 32 (27.12) | ||
| <15 points | 30 (53.57) | 86 (72.88) | ||
| ALB (g/l) | 4.698 | 0.035 | ||
| ≥30.0 | 21 (37.5) | 65 (55.08) | ||
| <30.0 | 35 (62.5) | 53 (44.92) | ||
| Use time of ventilator | 6.890 | 0.009 | ||
| ≥7d | 38 (67.86) | 55 (46.61) | ||
| <7d | 18 (32.14) | 63 (53.39) |
Table 2: Comparison of Various Parameters Between VAP Group and non-VAP Group
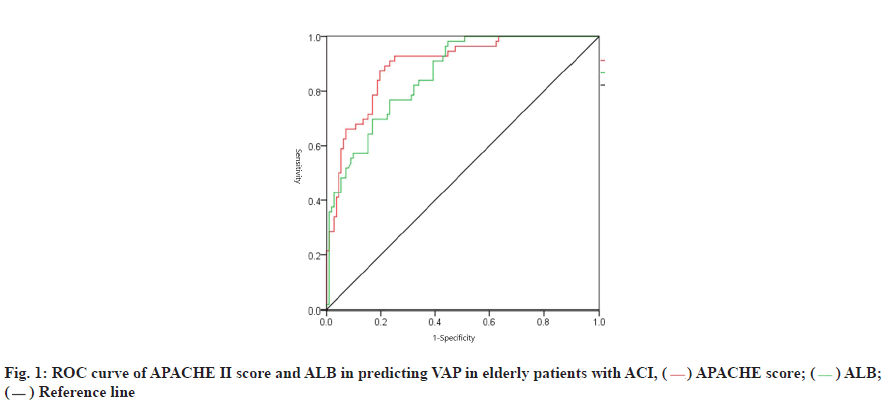
The value of APACHE II score and ALB in predicting VAP in elderly patients with ACI is given below. Receiver Operating Characteristic (ROC) curve was drawn. The results showed that the sensitivity of APACHE II score predicting VAP of patients with ACI was 93.71 %, the specificity was 77.61 % and the Area under the Curve (AUC) was 0.894. The sensitivity of ALB in predicting VAP of patients with ACI was 78.51 %, the specificity was 76.92 % and the AUC was 0.857 (Table 3 and fig. 1).
| Index | Cutoff value | Sensibility | Specificity | Missed diagnosis rate | Misdiagnosis rate | AUC value |
|---|---|---|---|---|---|---|
| APACHE II score | 15 | 93.71 | 77.61 | 6.29 | 22.39 | 0.894 |
| ALB (g/l) | 30 | 78.51 | 76.92 | 21.49 | 23.08 | 0.857 |
Table 3: The Value of Apache II Score and ALB in Predicting VAP in Elderly Patients With ACI
Logistic multivariate analysis with the occurrence of VAP as the dependent variable and the statistically significant index in the result of pathogenic bacteria status of 56 patients with VAP as the independent variable showed that the prophylactic ACI of antibacterial drugs and the high level of serum ALB could effectively reduce the risk of VAP of the elderly patients undergoing endotracheal intubation and mechanical ventilation (p<0.05) and the prolonging of the time of ventilator use and the increased APACHE II score was associated with an increased risk of VAP in the elderly patients with ACI undergoing endotracheal intubation and mechanical ventilation (p<0.05) (Table 4).
| Parameter | Beta (b) | SE | Wald’s test | p | Odds Ratio (OD) | 95 % Confidence Interval (CI) | |
|---|---|---|---|---|---|---|---|
| Prophylactic use of antimicrobials | -0.554 | 0.206 | 7.232 | 0.004 | 0.575 | 0.384 | 0.861 |
| APACHE II score | 0.818 | 0.361 | 5.134 | 0.037 | 2.266 | 1.117 | 4.598 |
| ALB | -0.207 | 0.085 | 5.931 | 0.021 | 0.813 | 0.688 | 0.960 |
| Use time of ventilator | 1.207 | 0.438 | 7.594 | 0.001 | 3.343 | 1.417 | 7.889 |
| Constant term | 1.443 | 0.613 | 5.541 | 0.032 | 4.233 | 1.273 | 14.076 |
Table 4: Multivariate Analysis of VAP Group
ACI is one of the most common cerebrovascular diseases in the elderly population. Among all cerebrovascular diseases, the proportion of ACI is 80 %. The pathogenesis of ACI is complicated, which is closely related to inflammatory reaction, abnormal lipid metabolism and hemodynamic changes. The pathogenesis is caused by blood supply disorder in brain, energy metabolism disorder resulting in cerebral ischemia, hypoxia necrosis and neurological impairment and thus prone to complications such as nerve damage [9-11]. ICU is a special area for rescue and monitoring of critically ill patients. The critical patients are concentrated, the basic diseases are serious, the space is relatively small and nosocomial infection is easy to occur. When the ventilator is used, it is necessary to establish an artificial airway, which can impair normal respiratory defenses [12]. The respiratory tract is directly connected to the outside world and does not act as a purifying agent of the upper respiratory tract for inhaled gases, so the incidence of VAP is high [13].
The results of pathogenic bacteria culture in this study showed that Gram-negative bacteria were the main pathogen, accounting for 67.86 %, followed by Grampositive bacteria accounting for 26.79 %. The study results showed that when comparing each index of VAP group and non-VAP group, there was no significant difference in age, gender, BMI, smoking, alcohol consumption, hypertension, diabetes and coronary heart disease between VAP group and non-VAP group; there was statistically significant difference in antimicrobial prophylaxis, time of ventilator use, APACHE II score and serum ALB level between VAP group and non-VAP group. The results showed that the use of antimicrobials, time of ventilator use, APACHE II score and serum ALB level could be used as early predictors of ACI with VAP in the elderly. This may be due to the long-term use of the ventilator in ICU patients, where incision of the trachea into the ventilator is required, resulting in an invasive injury that compromises the integrity of the mucosal epithelium of the respiratory tract. On the other hand, the endotracheal tube also stimulates the upper respiratory tract to produce more secretions and the accumulation of secretions accelerates the propagation of bacteria. The use of ventilator can prolong the mechanical ventilation time, resulting in the loss of humidification and bacterial filtration in the upper respiratory tract of human body, leading to dehydration of airway, dry airway mucosa and unsmooth drainage, so that bacteria enter the respiratory tract then retrograde into the condensed water of ventilator catheter and meanwhile, long-term mechanical ventilation also increases the possibility of pathogens invading into human body. Antimicrobial agents are commonly used to elevate the pH of the human stomach, weaken the body’s killing of pathogenic bacteria that enter the stomach and cause VAP by reflux or aspiration of the esophagus [14]. Logistic multivariate analysis in VAP with the occurrence of VAP as the dependent variable and the statistically significant index as the independent variable showed that the prophylactic ACI of antibacterial drugs and the high level of serum ALB could effectively reduce the risk of VAP of the elderly patients undergoing endotracheal intubation and mechanical ventilation and the prolonging of the time of ventilator use and the increased APACHE II score was associated with an increased risk of VAP in the elderly patients with ACI undergoing endotracheal intubation and mechanical ventilation. ROC curves were drawn. The results showed that APACHE II score and ALB prediction can well predict the sensitivity and specificity of VAP in patients with ACI, with good predicting value.
Studies on various aspects have gained increasing attention in China in recent years. However, most studies on surgical ICUs are retrospective and use statistical methods to describe descriptive methods or univariate analyses [15,16]. In this study, we used unconditional regression model analysis to identify more closely related risk factors from various risk factors and conducted in-depth analyses of the interactions among these factors to identify susceptible population indications, identify key surveillance goals, develop targeted preventive care strategies and provide basic epidemiological data for the prevention and treatment of surgical ICUs.
In conclusion, there are many factors influencing the occurrence of VAP in the elderly patients with ACI undergoing endotracheal intubation and mechanical ventilation and the intervention according to the risk factors has a positive preventive effect. In clinical practice, it is necessary to shorten the time of ventilator use, reasonably control the use of antibacterial drugs, timely observe the patient’s condition and correct the phenomenon of regurgitation and aspiration, reduce the infection rate of VAP and improve the therapeutic effect.
Conflict of interests:
The authors declared no conflict of interest.
References
- Lewis RH, Sharpe JP, Swanson JM, Fabian TC, Croce MA, Magnotti LJ. Reinventing the wheel: Impact of prolonged antibiotic exposure on multidrug-resistant ventilator-associated pneumonia in trauma patients. J Trauma Acute Care Surg 2018;85(2):256-62.
- Johnstone J, Heels-Ansdell D, Thabane L, Meade M, Marshall J, Lauzier F, et al. Evaluating probiotics for the prevention of ventilator-associated pneumonia: A randomised placebo-controlled multicentre trial protocol and statistical analysis plan for prospect. BMJ Open 2019;9(6):e025228.
- Chang L, Dong Y, Zhou P. Investigation on risk factors of ventilator-associated pneumonia in acute cerebral hemorrhage patients in intensive care unit. Can Respir J 2017;2017.
- Simmons JD, Freno DR, Muscat CA, Obiako B, Lee YL, Pastukh VM, et al. Mitochondrial DNA damage associated molecular patterns in ventilator-associated pneumonia: Prevention and reversal by intratracheal DNase I. J Trauma Acute Care Surg 2017;82(1):120-2.
- Burja S, Belec T, Bizjak N, Mori J, Markota A, Sinkovi? A. Efficacy of a bundle approach in preventing the incidence of ventilator associated pneumonia (VAP). Bosn J Basic Med Sci 2018;18(1):105-9.
- VandanaKalwaje E, Rello J. Management of ventilator-associated pneumonia: Need for a personalized approach. Expert Rev Anti Infect Ther 2018;16(8):641-53.
- Agrawal GN, Shevade SU. Comparison of Clinical and Laboratory Standards Institute 2008 and 2010 guidelines in interpreting susceptibility of enterobacteriaceae isolates. Indian J Pathol Microbiol 2014;57(3):518-9.
- Godinjak A, Iglica A, Rama A, Tan?ica I, Jusufovi? S, Ajanovi? A, et al. Predictive value of SAPS II and APACHE II scoring systems for patient outcome in a medical intensive care unit. Acta Med Acad 2016;45(2):97-103.
- Millot G, Voisin B, Loiez C, Wallet F, Nseir S. The next generation of rapid point-of-care testing identification tools for ventilator-associated pneumonia. Ann Transl Med 2017;5(22):451-2.
- Yu Y, Zhu C, Liu C, Gao Y. How to remove the grey area between ventilator-associated pneumonia and ventilator-associated tracheobronchitis? Crit Care 2017;21(1):1-2.
- Kózka M, Sega A, Wojnar-Gruszka K, Tarnawska A, Gniadek A. Risk factors of pneumonia associated with mechanical ventilation. Int J Environ Res Public Health 2020;17(2):656.
- Letchford E, Bench S. Ventilator-associated pneumonia and suction: A review of the literature. Br J Nurs 2018;27(1):13-8.
- Ergul AB, Cetin S, Altintop YA, Bozdemir SE, Ozcan A, Altug U, et al. Evaluation of microorganisms causing ventilator-associated pneumonia in a pediatric intensive care unit. Eurasian J Med 2017;49(2):87-8.
- Nair GB, Niederman MS. Using ventilator-associated pneumonia rates as a health care quality indicator: A contentious concept. Semin Respir Crit Care Med 2017;38(3):237-44.
- de Silva NL, Gooneratne L, Wijewickrama E. Acute myocardial infarction associated with thrombotic microangiopathy following a hump-nosed viper bite: A case report. J Med Case Rep 2017;11(1):1-7.
- DeLuca Jr LA, Walsh P, Davidson Jr DD, Stoneking LR, Yang LM, Grall KJ, et al. Impact and feasibility of an emergency department-based ventilator-associated pneumonia bundle for patients intubated in an academic emergency department. Am J Infect Control 2017;45(2):151-7.
 ) APACHE score; (
) APACHE score; ( ) ALB; (
) ALB; ( ) Reference line
) Reference line



