- *Corresponding Author:
- B. Zhang
Department of Plastic Surgery, The First Hospital of Shanxi Medical University, Taiyuan City, 030001, Shanxi Province, China
E-mail: zhangbaolin4007@126.com
| This article was originally published in a special issue, "Clinical and Experimental Studies on Drug and Intervention Repurposing in China |
| Indian J Pharm Sci 2019:81(4)spl issue1;144-150 |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
In order to study the repairing effects of aesthetic surgery technology on patients with facial trauma, patients with facial trauma were taken as the research subjects. Through the observation of postoperative pigmentation (M), vascularity (V), height (H), and pliability (P) of patients with trauma on the lower faces who received aesthetic surgery treatments, the contrast before and after the surgeries as well as the satisfaction were analyzed and investigated. The results showed that aesthetic surgery technology has a significant effect on the recovery of postoperative indices in patients with facial trauma. In addition, the factors that would affect the postoperative recovery of patients were also analyzed. In summary, aesthetic surgery treatments have good effects on the recovery of patients with facial trauma, which can greatly improve the psychological recovery of patients to maintain their confidence in work and life. Despite the deficiencies in the research process, it has provided a certain basis and ideas for subsequent research. Therefore, the study is of great significance.
Keywords
Face, recovery, cosmetology, surgery
The face is a body part where organs and structures are very concentrated. At the same time, it is a body part with very high aesthetic requirements[1]. Unlike other body parts, the face is often exposed to the external environment; thus, it is easy to receive damages, causing skin lacerations, tissue defects, and damages to the organ structure[2]. The repair method of human tissue after trauma is scar repair; however, the patient is often treated in the emergency department after the injury, where the doctor lacks understanding of aesthetic surgery suture techniques and the emergency department does not have the fine equipment needed for aesthetic surgery, thus, the aesthetic effects and requirements of face trauma recovery cannot be achieved. Therefore, how to reduce the post-recovery scar has become a major concern[3,4]. With the improvement of living standards, the aesthetic requirements of people are very high. Patients with facial trauma not only require wound healing but also wish to look beautiful. Improper treatments would leave obvious scars, resulting in scar hyperplasia, scar contracture, which not only affects the appearances of patients but also may cause local tissue and structures to displace and deform, and even severe psychological problems[5,6]. Skin is the largest organ of the human body, containing many layers and cells. After injury, after a series of processes in the wound such as the accumulation of inflammatory cells, the release of growth factors, cell proliferation and differentiation, collagen production, and apoptosis of cells such as fibroblasts, the original normal skin is replaced by granulation tissues and then by scar tissues[7]. On the face, scars not only affect the appearances but also the functions of the organs in key areas, and even could seriously affect the mental health of patients[8,9].
After the improvement in material levels, the desire for beauty of people is increasing; patients would seek wound healing along with reduction of or even elimination of scars. Although wound healing and scar treatments have gradually advanced to molecular and genetic levels, the current technology cannot eradicate scars[10]. However, many injured patients were treated with techniques and materials of aesthetic surgery in the first phase, whose scars were lighter and had less impact on their appearances, functions, and psychological status after the wounds were healed[11]. Therefore, a total of 223 patients with facial trauma who were treated with aesthetic and cosmetic techniques in the Department of Aesthetic Surgery were followed up, and the cases of 48 patients with facial sutures who received ordinary facial sutures were collected[12]. Scars of these patients were evaluated, and the degree of satisfaction of both doctors and patients were surveyed and compared[13]. Through these evaluations and comparisons, the therapeutic effects of early aesthetic surgery treatments on patients with facial trauma were observed, the preventions and early active treatments of scars were explored, thereby improving the postoperative appearances and reducing the psychological burdens of patients, as well as improving the quality of life of patients[14].
In summary, the effects of facial repair on patients with facial injuries after undergoing aesthetic surgery treatments were analyzed. The results showed that aesthetic surgery treatments exhibited good wound repair in patients with facial injuries. The innovation of this study is to analyze the whole aesthetic repair process from the perspective of preoperative evaluation, the repair process, and the postoperative investigation. Despite the deficiencies in the research process, it has provided a certain basis and ideas for subsequent research.
A total of 100 patients with facial soft tissue injuries treated in the Department of Aesthetic Surgery of a hospital from January 1 to June 31, 2017 were recorded and followed up. First, patients with concomitant organ injuries (cranial, intra-abdominal) or unstable vital signs, who were transferred to specialist treatment; second, patients who suffered from systemic diseases that could affect the wound healing (such as diabetic patients with poor plasma glucose control, renal dysfunction, malignant tumors, immune system diseases, malnutrition, metabolic diseases); third, patients who took hormones for a long time or received radiotherapy or chemotherapy were excluded.
Preoperative evaluations performed were, since the face of patients was exposed to the external environment, it was more likely to be injured than other body parts and may cause damages to other body parts. Therefore, before the facial surgeries were performed, the vital parameters of patients were evaluated; then, the doctors should communicate with the patients in detail, including asking the patients about their current and previous medical histories; besides, through the communications and conversations, the possibility of craniocerebral injury of patients should be determined; in addition, the cause of their facial injuries should also be investigated to determine the residual impurities and contamination of the wounds; if the patient was injured within 48 h, the stage I debridement and suture treatments could be given, and then a preliminary examination of the wound was carried out to further determine whether the patient had a fracture or damage to other vital organs. If necessary, patients should be submitted to X-ray computed tomography (CT), magnetic resonance imaging (MRI), and other imaging examinations. A large number of studies have shown that facial trauma is accompanied by craniocerebral injury, and the combined brain injury is an important cause of death in patients with facial injuries. Therefore, clinically, in foreign countries, patients with facial injuries were generally diagnosed by multi-disciplinary cooperation, such as the cooperation with Department of Ear, Nose, and Throat and the Department of Oral and Maxillofacial Surgery; the multi-disciplinary cooperation diagnosis could ensure that every damage to the patient can get the most reasonable treatment, and thus may get a more perfect effect. If the patient was found to have other symptoms such as malnutrition, diabetes, and other additional diseases during the consultation, it should be more cautious during the operation.
Preoperative preparations included, before the surgeries, it was necessary to ensure that excellent medical equipment was prepared for the surgeries; in addition, the conditions and the expected effects of the surgeries should be fully explained to the patients and the patients can only be operated after their consent was obtained. Studies have shown that doctors tend to be satisfied with the expected results of the surgical results that can be achieved after surgeries. However, patients may be unsatisfied with the results of surgeries for some reasons. It was observed that the wound was generally repaired by scar tissues according to the current study; however, these repairing tissues generally existed only in younger patients, which was a large cause of the gap between the expectations of patients and doctors. Thus, it was necessary to give the patients a clear explanation before surgeries.
If the patients had only soft tissue damage of the face without any damages to the key organs or tissues and if their vital parameters were normal and stable, the surgeries to be conducted with partial infiltration anesthesia; the preparation of local anesthetics was 3 % lidocaine and adrenal hormones (the ratio was 1:100 000). The addition of adrenal hormone could promote vasoconstriction, thereby reducing bleeding and oozing during surgery, creating a clean environment for the normal operations of the surgeries. Another effect of adding adrenal hormone was to increase the effect of anesthesia on the patients and to reduce systemic side effects of the local anesthetics as much as possible.
For debridement of patients who were treated in the Department of Aesthetic Surgery, the rules and regulations of surgical debridement and suture have been followed, and the key points of aesthetic surgery and suture must be noted. The specific operative steps were, firstly, cleaning the skin near the wound, covering with wet sterile gauze, preparing the specific skin near the wound, removal of useless tissue that disturb the surrounding area, and cleaning the nearby skin with distilled water; then, the wound was cleaned repeatedly with saline, most importantly, the interfering substances such as impurities and dirt near the wound should be cleaned; under normal circumstances, cleaning was repeated at least 5 times followed by 2.8 % povidone-iodine solution was used to repeatedly rinse around the wound to remove the stain for at least 5 times, which was at least 20 cm away from the wound; afterwards, a sterile towel was placed on the top of the wound. Secondly, local infiltration anesthesia with 3 % lidocaine; after the anesthesia was completed, 2 % H2O2+saline was used to repeatedly rinse the wound for at least 5 times; then, the wound was rinsed with diluted povidone-iodine solution and saline alternatively for at least 5 times; afterward, the liquid around the wound was cleaned with sterile gauze, the wound was carefully inspected, and all the impurities and foreign matters left in the wound were removed; if the patient presented significant hemorrhage, the electric coagulation and ligation was used to control the hemorrhage to protect the critical organ tissues; the ineffective tissue cells were removed; the wound was consequently sutured with angle needles and 3-0 and 4-0 black silk threads in the whole layer interrupted sutures. After the suture, the wound was gently turned outward and wrapped with sterile gauze.
During the interrupted suturing of tissues, it should be noted that the needle must penetrate deep epidermis from the side of the wound and go out from the shallow epidermis; next, the needle must go in the shallow epidermis from the other side of the wound and go out from the deep epidermis, followed by tying the knot; it should be noted that the shallow knot must be tied in the deep layer of the tissue), the tension should be reduces as much as possible (before the suture of the epidermis, the edge of the wound would be self-recovered without the promotions of external forces). The sutures must be performed layer by layer (the dermis layer, the periosteum layer, the subcutaneous tissue layer, and the muscular layer), the suture of each needle must ensure that the slice thickness of skin on both sides was the same, and the incomplete suture due to the dislocation of the tissue must not occur. Afterward, the epidermis was disinfected by 2.8 % povidone-iodine solution, the epidermis was sutured by interrupted sutures with nylon threads, the tension must be kept appropriate, the epidermis should be slightly flipped outward (3 mm from the edge and 5 mm from the needle) or glued with medical glue. Patients with skin tissue loss could be treated with the partial cutaneous flap treatment (rotary cutaneous flap and propulsion cutaneous flap). If loss of skin in patients was relatively severe, which could not be repaired by the partial cutaneous flap, the transplant treatment with full-thickness or moderate-thickness flap should considered. Generally, the skin behind the ears or at the inner side of the forearm was used. After the suture was completed, the recombinant bovine fibroblast growth factor gel was re-applied; the wound was covered with gauze and then wrapped with sterile gauze. In terms of patients who were treated in the emergency department, the rules and regulations for surgical debridement and suture should be followed. The specific operative methods were, firstly, cleaning the skin near the wound, the wound was covered with wet sterile gauze, the specific skin near the wound was prepared, the useless tissue that disturbed the surrounding area was removed, and the nearby skin was cleaned with distilled water; then, the wound was cleaned repeatedly with saline, most importantly, the interfering substances such as impurities and dirt near the wound should be cleaned; under normal circumstances, the cleaning was repeated for at least 5 times; next, the 2.8 % povidone-iodine solution was used to repeatedly rinse around the wound to remove the stain for at least 5 times, which was at least 20 cm away from the wound; afterwards a sterile towel was placed on the top of the wound; secondly, local infiltration anesthesia, the 3 % lidocaine was used for local anesthesia; after the anesthesia was completed, the 2 % H2O2+saline was used to repeatedly rinse the wound for at least 5 times; then, the wound was rinsed with diluted povidone-iodine solution and the saline alternatively for at least 5 times; afterward, the liquid around the wound was cleaned with sterile gauze, the wound was carefully inspected, and all the impurities and foreign matters left in the wound were removed; if the patient was accompanied by significant hemorrhage, the electric coagulation and ligation would be utilized to control the hemorrhage to protect the critical organ tissues; the ineffective tissue cells were removed; the wound was consequently sutured with angle needles and 3-0 and 4-0 black silk threads in the whole layer interrupted sutures.
After the suture, the wound was gently turned outward and wrapped with sterile gauze. Postoperative treatments within 48 h after the injury, the tetanus antitoxin skin test should be carried out in the emergency department. If the patient was allergic, the tetanus immunoglobulin should be utilized for testing. Respectively on d 2, 4 and 6 after the surgery, the dressings and drugs should be changed; if there was excessive secretion of fluid in the wound, the dressings and drugs should be changed every day for the first 3 days after surgery. In general, the sutures to be removed 1 w after the surgery. In terms of patients with dark cutaneous flaps and poor blood circulation, the high-pressure oxygen treatments were required every day for the first 3 d after surgery; the subcutaneous hematoma and exudate should be removed as soon as possible; 5 d after the completion of the suture removal, based on their personal conditions, patients could apply the antiscar hyperplasia products as needed. In terms of patients whose wounds were healed under normal conditions, if their requirements on scar recovery were relatively higher, the fractional laser treatments could be utilized for further recovery treatments 10 mo after the surgeries when the scars were stable. In terms of patients who were sensitive to scars or had the tendencies of scar hyperplasia, the separate or joint treatments of local radiotherapy, elastic sleeve compression treatment, and hormone injections into the scars should be given as soon as possible. For patients who were treated in the emergency department within 48 h after the injury, the procedure as described for postoperative treatments should be carried out in the emergency department.
The recovery of aesthetic surgery wounds is an extremely complicated and regular process, which includes 3 major processes, which are, first, the most important process is the first stage in which the hemorrhage is stopped and the inflammation is eliminated, followed by the process of cell proliferation and fission, and the final process is the reorganization of epidermis and presence of scars. Current research on these processes range from the cellular level to the molecular level, even the genetic level, and the whole process involves multiple types of cells and factors. In addition, the rehabilitation of the wound is affected by many other factors (such as wound cleanliness, blood supply, impurities, oxygen concentration, environmental temperature, environmental humidity, surgical mode, wound direction, tension, age and internal environment). The role of any section has a great impact on the prognosis.
All patients were followed up for 5 mo through telephone or clinical visits; telephone follow-ups were interviewed and recorded, and follow-up visits were performed by specialists.
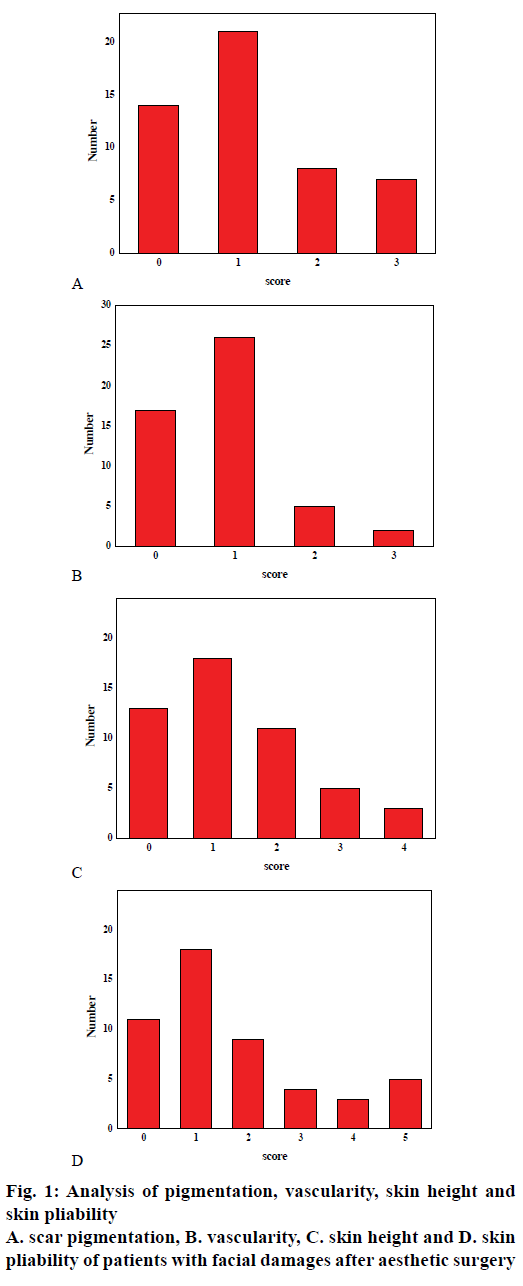
Firstly, referring to the Vancouver scar scale shown in Table 1, the pigmentation (0-3 points), vascularity (0-3 points), height (0-4 points), and pliability (0-5 points) of the scar were observed. The score was 0 points to the minimum and 15 points to the maximum. The higher the score, the heavier the scar. The points of each patient were independently scored by 2 doctors and the average was taken. Secondly, the degree of satisfaction of doctors and patients on post-recovery effects were surveyed.
| 0 points | 1 point | 2 points | 3 points | 4 points | 5 points | |
|---|---|---|---|---|---|---|
| Pigmentation (M) | Normal | Hypopigmentation | Mixed | Hyperpigmentation | ||
| Vascularity (V) | Normal | Pink | Red | Purple | ||
| Height (H) | Flat | 0<H<1 mm | 1<H<2 mm | 2<H<4 mm | H>4 mm | |
| Pliability (P) | Normal | Supple | Yielding | Firm | Ropes | Contracture |
Table 1: The vancouver scar scale
The analysis of scar pigmentation of patients with facial damages after aesthetic surgery treatments was shown in fig. 1. As can be seen from the figure, the scar pigmentation of patients with facial damages after aesthetic surgery treatments were mostly concentrated between 0-1, and the indicator analysis of the Vancouver Scar Scale indicated that the smaller the scores were, the better the skin recovery of patients was, and the closer to the standard requirements of normal skin the effects were. Therefore, it can be seen that aesthetic surgery has a good effect on the facial appearance recovery of patients with facial damages, which will greatly enhance the self-confidence of life and work of the patients. In addition, it fully proves that aesthetic surgery has a good ability to repair the facial appearances of patients with facial injuries in terms of the pigmentation of scars.
The vascularity of patients with facial damages after aesthetic surgery treatments is shown in fig. 1. As can be seen from the figure, in the recovery stage after surgical treatments, the vascularity of patients was mainly concentrated between 0-1, and the indicator analysis of the Vancouver Scar Scale indicated that the smaller the scores were, the much closer to the normal skin the skin was. Therefore, it can be seen that as small as the scores 0-1 were, the aesthetic surgery treatments have an improved effect on the vascularity of the facial appearances in patients with facial damages. The skin height of patients with facial damages after aesthetic surgery treatments was shown in fig. 1. As can be seen from the figure, patients whose scores were 0 and 1 accounted for about 75 %, and patients whose scores were 2, 3, 4 accounted for about 25 %. The smaller the score was, the better the skin recovery was. Therefore, it can be seen that aesthetic surgery treatments have a positive influence on the skin height of patients with facial damages.
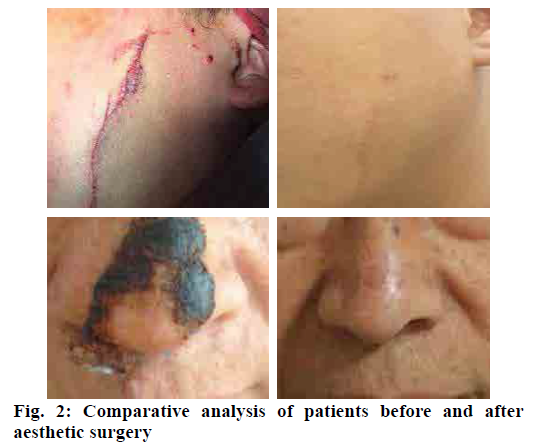
Comparative analysis of patients before and after aesthetic surgery treatments was shown in fig. 2. As can be seen, the changes of the patients before and after the repairing surgeries were very obvious; the previous scars and repair marks were almost invisible, and the empirical photos were sufficient enough to illustrate that the aesthetic surgery treatments have a good effect on the facial appearance recovery of patients with facial damages.
The skin pliability of patients with facial damages after aesthetic surgery treatments was shown in fig. 1. Combined with the indicators of Vancouver Scar Scale and the data in the graph, it could be analyzed that the recovery of patients after surgeries showed that the majority of patients had positive recovering effects; however, some patients were unsatisfactory with their recovering effects and needed follow-up observations. The reason was that the personal conditions and wounds of patients were different. In general, aesthetic surgery has a good effect on the recovery of skin pliability in patients with facial damages.
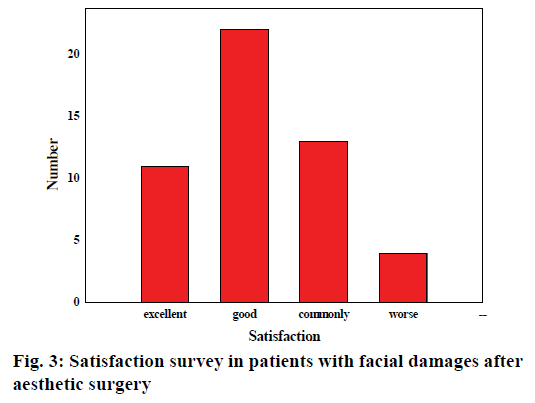
The satisfaction survey of patients with facial damages after aesthetic surgery treatments was shown in fig. 3. It can be seen from the data distribution in the figure that most patients were highly satisfied with the postoperative effects, most of which were very good or good. The personal reflections and feedback of patients were enough to indicate the degree of satisfaction of the postoperative effects, and 70 % of patients were satisfied with the results, which could prove the therapeutic effects of aesthetic surgery treatments.
Influencing factors and repairing effects of aesthetic surgery technology on patients with facial trauma were explored and investigated. Through the observation of postoperative indicators such as pigmentation, vascularity, height, pliability, comparison between the preoperative and postoperative images, and the satisfactions were analyzed and investigated in detail. The results showed that aesthetic surgery technology has a significant effect on the facial wound recovery in patients with facial trauma, which can greatly improve the self-confidence of patients. However, certain deficiencies were found in the research process, such as the sample capacity was not large enough, the wound site and condition of each patient were different, and the physical condition of each patient was different. Despite the deficiencies in the research process, it has provided a certain basis and ideas for subsequent research on aesthetic surgery recovering treatments.
References
- Kim Y, Kim H, Kim YO. Virtual reality and augmented reality in plastic surgery: a review. Arch Plast Surg 2017;44(3):179.
- Moubayed SP, Ioannidis JPA, Saltychev M, Most SP. The 10-item Standardized Cosmesis and Health Nasal Outcomes Survey (SCHNOS) for functional and cosmetic rhinoplasty. JAMA Facial Plast Surg 2018;20(1):37-42.
- Kanevsky J, Corban J, Gaster R, Kanevsky A, Lin S, Gilardino M. Big data and machine learning in plastic surgery: a new frontier in surgical innovation. Plast Reconstr Surg 2016;137(5):890e-897e.
- Harrar H, Myers S, Ghanem AM. Art or Science? An evidence-based approach to human facial beauty a quantitative analysis towards an informed clinical aesthetic practice. Aesthetic Plast Surg 2018;42(1):137-46.
- Patel K, Brandstetter K. Solid implants in facial plastic surgery: potential complications and how to prevent them. Facial Plast Surg 2016;32(05):520-31.
- Kamali P, Dean D, Skoracki R, Koolen PG, Paul MA, Ibrahim AM, et al. The current role of three-dimensional printing in plastic surgery. Plast Reconstr Surg 2016;137(3):1045-55.
- Golshani S, Mani A, Toubaei S, Farnia V, Sepehry AA, Alikhani M. Personality and psychological aspects of cosmetic surgery. Aesthetic Plast Surg 2016;40(1):38-47.
- Hsieh TY, Dedhia R, Cervenka B, Tollefson TT. 3D Printing: current use in facial plastic and reconstructive surgery. Curr Opin Otolaryngol Head Neck Surg 2017;25(4):291-9.
- Carruthers J, Burgess C, Day D, Fabi SG, Goldie K, Kerscher M, et al. Consensus recommendations for combined aesthetic interventions in the face using botulinum toxin, fillers, and energy-based devices. Dermatol Surg 2016;42(5):586-97.
- Vaca EE, Purnell CA, Gosain AK, Alghoul MS. Postoperative temporal hollowing: Is there a surgical approach that prevents this complication? A systematic review and anatomic illustration. J Plast Reconstr Aesthet Surg 2017;70(3):401-15.
- Pfaff MJ, Steinbacher DM. Plastic surgery applications using three-dimensional planning and computer-assisted design and manufacturing. Plast Reconstr Surg 2016;137(3):603e-16e.
- Damgaard OE, Larsen CG, Felding UA, Toft PB, von Buchwald C. Surgical timing of the orbital “blowout” fracture: a systematic review and meta-analysis. Otolaryngol Head Neck Surg 2016;155(3):387-90.
- Scheuer JF, Sieber DA, Pezeshk RA, Gassman AA, Campbell CF, Rohrich RJ. Facial danger zones: techniques to maximize safety during soft-tissue filler injections. Plast Reconstr Surg 2017;139(5):1103-8.
- Naraghi M, Atari M, Asadollahi H. When aesthetics, surgery, and psychology meet: aesthetic nasal proportions in patients having rhinoplasty and normal adults. Surg J 2016;2(01):e44-e48.