- *Corresponding Author:
- X. Zheng
Department of Obstetrics, Affiliated Hospital of Hebei University, No. 212, Yuhua East Road, Baoding, Hebei 071000, China
E-mail: zhengxian1897@sina.com
| This article was originally published in a special issue,“Evolutionary Strategies in Biomedical Research and Pharmaceutical Sciences” |
| Indian J Pharm Sci 2020:83(3)Spl issue;36-41 |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
The aim of this study was to investigate the effect of ergonovine combined with spiral suture of lower uterine segment in the treatment of pernicious placenta previa hemorrhage after cesarean section. A retrospective analysis of the clinical data of 74 patients hospitalized in our hospital due to pernicious placenta previa from January to February 2016, divided them into a study group and a control group. The study group included 37 patients who received ergonovine injection into the lower uterine muscle wall+spiral suture of the lower uterus during cesarean section, and the control group included 37 cases who received the conventional method and row suture of the lower uterus. The blood loss during operation, 2 h after operation and 2-24 h after operation, operation time, hysterectomy rate, postoperative uterine involution and incision healing were observed. The systolic and diastolic blood pressure, pulse level and the incidence of postoperative complications were compared between the two groups. The results showed that the combined application of ergonovine and lower uterine spiral suture was effective in treating pernicious placenta previa hemorrhage after cesarean section. It was a simple, easy, safe and reliable surgical hemostasis method, which could effectively control massive bleeding during the operation, avoid the removal of the uterus, and completely remove the placenta and restored the shape of the lower part of the uterus by ring-shaped narrowing, which helped the uterus to regenerate after delivery.
Keywords
Pernicious placenta previa, suture technique, ergonovine
Placenta previa is a clinically common obstetric complication, which mostly occurs in the late pregnancy [1]. Pregnant women with placenta previa are prone to vaginal bleeding. Clinically, placenta previa is divided into pernicious placenta previa (PPP) and non-dangerous placenta previa [2]. PPP refers to the placenta attached to the scar of the previous cesarean section, or the placenta previa with placenta accreta or placental adhesions. Relevant data show that the risk of placental implantation is 50 %, which may lead to intraoperative and postoperative bleeding that is difficult to control during cesarean section, which may cause hemorrhagic shock and diffuse intravascular coagulation, endangering the life of the mother and increase perinatal hysterectomy rate [3-5]. With the opening of the two-child policy, it is foreseeable that the cesarean section rate, which was as high as 50 % in China, will cause a huge number of PPP parturients, and how to deal with the intraoperative bleeding is one of the most pressing problems for obstetricians in China [6,7].
PPP parturients often suffer catastrophic hemorrhage when the placenta tissue is removed after delivery of the fetus, which is a common cause of hysterectomy. Obstetricians at home and abroad have proposed a variety of uterine suture methods. In our department, ergonovine+lower uterine spiral suture was used in combination, which achieved good therapeutic effects in our hospital and some medical units and improved the outcome of mother and child [8].
Materials and Methods
Data collection:
A total of 74 patients with PPP who underwent cesarean section were selected from our hospital from January 2016 to September 2018, aged 20-40 y old, with an average age of 30.15±5.26 y old; gestational age 25 -40 w, average gestational age 35.122.48 w.
These patients were aged 20-40 y old, with an average age of 30.15±5.26 y old, pregnant 25-40 w, with an average gestational age of 35.12±2.48 w. Among them, there were 25 cases of primiparous women and 49 cases of postpartum women. The anterior type: 46 cases of central type, 16 cases of edge type, and 12 cases of partial type. According to the random number method, all patients were divided into observation study group and control group, with 37 cases in each group. Among them, 37 patients who used ergonovine lower uterine muscle wall injection+lower uterine spiral suture were the study group, and the remaining 37 cases who used conventional methods and lower uterine row suture were the control group. All 74 PPP parturients underwent three-dimensional ultrasonography before operation and recorded the placenta attachment site, cervical canal length, placental blood flow, and the relationship between placenta and bladder. All patients and their families were informed about this study, and they had signed an informed consent form.
Research method:
The patient was placed in the supine, and sets a collector under the hip to collect vaginal bleeding. This position would be convenient for intraoperative vital signs monitoring, blood transfusion, observation of patients vaginal bleeding, and could also be used for transvaginal sutures when necessary. After opening the peritoneum, first explore the right rotation of the uterus to understand the main attachment sites of the placenta, and whether there is placental penetration or implantation. Palpate to find the most accessible and weakest area of the uterus, try to avoid the placenta, and cut the uterus in a horizontal arc, L-shape or V-shape at the edge of the placenta.
The fetus in the control group was immediately injected with 250 μg carboprost tromethamine into the lower uterine muscle wall after delivery. After the placenta was delivered, 10 units of oxytocin were given into the pot and 10 units into the liquid. If there was extensive blood oozing on the peeling surface, row suture was performed immediately. After the placenta was delivered, 10 units of oxytocin were given into the pot and 10 units into the liquid. If there was extensive blood oozing on the peeling surface, row suture was performed immediately.
Pulled the uterus out of the abdominal cavity, used both hands to compress the lower part of the uterus, pushed down the bladder and fold the peritoneum to the lower part of the internal cervix. using the absorbable catgut to absorb the gut. The first needle insertion point was 4-5 cm from the lower edge of the anterior wall of the uterus and 2-3 cm from the right edge of the uterus, and the needle insertion point was as close as possible to the level of the internal cervix, and the suture penetrated the uterus vertically. Then the needle was drawn from the serosal layer of the posterior wall of the uterus, vertically upwards, and inserted in the posterior wall of the uterus at 3 cm of the upper edge of the incision on the anterior wall of the uterus. The upper and lower needle insertion options for the left side incision on the anterior wall of the uterus were symmetrical with the needle insertion points on the right side of the uterus. Tighten the left and right sutures at the same time under the pressure of the assistant. After observing that there was no active bleeding in the uterus, tighten the knots and closed the uterine incision. Observed for 15-30 min after suture to confirm that the uterus was ruddy in color, contraction became hard, vaginal bleeding stopped, and vital signs were stable, and then the abdomen could be routinely closed, and broad-spectrum antibiotics should be used to prevent infection after surgery.
After the fetus in the research group was delivered, the placenta was temporarily removed, and the operation was carried out according to the following steps. Exposure: There was no serious adhesion in the pelvic cavity, pulled the bottom of the uterus so that the uterus was completely outside the abdominal cavity, and wrapped the uterus with wet gauze to protect the uterus before proceeding. The uterine incision was clamped with non-toothed ring forceps, and the uterine swelling and expansion, the loss of the anterior wall of the lower uterus, and the adhesion of the bladder were carefully examined from the front and back. Clamping the bilateral uterine arteries: Placed sand clamps in the avascular area of the broad ligaments on both sides with adequate blood preparation and clamped the descending branches of the bilateral uterine arteries until the end of the suture on the inner side of the uterine cavity. Removal of placental tissue: The combination of blunt separation and sharp separation was used to quickly and thoroughly remove placental tissue, especially at the lower uterine segment near the cervix, so as to achieve no placental tissue residue. Multi-directional spiral suture of the lower uterus: The inner side of the lower uterine cavity was divided into four areas, anterior, posterior, left, and right, and in each area from the mucosa to the serosal surface, from the bottom (cervix uterus) to the top (uterine cavity), continuous and rapid transversely constricted sutures, the lower edge reached the plane of the inner cervix, and the upper edge exceeded 1 cm above the active bleeding point. In the 4 areas of the lower uterus, due to different placental attachment sites, adhesions, and implantation conditions, intraoperative bleeding was also different. One case with turbulent bleeding should be used as the starting area for suture. Preoperative imaging examination could indicate the most abundant blood supply (blood supply) or suspected placental implant site, which could help to determine the initial suture area during the operation. After suturing one area, it was necessary to observe the bleeding and decide whether other areas need to be sutured. Usually, 1-3 areas were sutured, and 4 areas were sutured if necessary. Choose 1-0 absorbable sutures and control the depth of suture not to exceed the uterine serosal layer, if the front wall was thin and adheres closely to the bladder, tried to avoid penetrating the bladder mucosa. Inspection and reinforcement: Removed the sand forceps and checked whether there was active bleeding in the cervix and/ or uterine cavity from the uterine cavity surface and vaginal surface. If necessary, re-stabilize the inside or surface of the uterus with patch sutures, or added supplementary surgical hemostasis.
Observation and follow-up:
We analyzed the amount of blood loss during the operation, the amount of bleeding after 2 h, the amount of bleeding after 2-24 h, the number of hysterectomies, the operation time, the duration of postoperative bloody lochia, and the recovery time of menstruation and performed routine gynecological examination and pelvic ultrasound 42 d after the operation to understand the involution of the uterus and the healing of the uterine incision.
Statistical processing:
Statistical software, statistical package for the social sciences (SPSS) 22.0 was used to analyze the data. Measurement data conforming to normal distribution were expressed as mean standard deviation (χ±s), and t test was used for comparison between groups. Enumeration data were expressed as case number (n) or percentage (%), and χ2 test was used to compare. The difference was statistically significant when p<0.05.
Results and Discussion
The general data comparison results of the two groups are shown in Table 1. There was no significant different in age, gestational weeks, body mass index (BMI), type of pregnant woman and type of placenta between the two groups (p>0.05).
| Group | Observation group (n=37) | Control group (n=37) | Statistics | p value |
|---|---|---|---|---|
| Average age (y) | 28.45±2.06 | 28.15±2.16 | 6.297 | 0.124 |
| Average gestational w (w) | 35.89±3.16 | 35.15±3.24 | 6.003 | 0.492 |
| BMI (kg/m2) | 22.15±2.48 | 22.31±2.46 | 5.239 | 1.004 |
| Type of pregnant woman | 6.497 | 1.037 | ||
| Initial pregnant women | 12 | 13 | ||
| Pregnant women | 25 | 24 | ||
| Type of placenta | 6.229 | 1.268 | ||
| Central | 23 | 23 | ||
| Partial | 6 | 6 | ||
| Edge type | 8 | 8 |
Table 1: Comparison of General Data Between the Two Groups
The surgical results of the two groups were compared with those in Table 2. The blood loss, 2 h, 2-24 h, hysterectomy and operation time in the study group were significantly lower than those in the control group (p<0.05), but there was no significant difference between the study group and the control group (p>0.05).
| Group | N | Intraoperative bleeding (ml) | Postoperative bleeding 2 h (ml) | 2-24 h bleeding after operation | Hysterectomy (case) | Operation time (min) | Blood lochia time (d) | Menstrual recovery time (mo) |
|---|---|---|---|---|---|---|---|---|
| Study group | 37 | 538.6±218.7 | 54.2±3.6 | 292.0±96.5 | 0 | 52.2±18.4 | 7.4±4.1 | 7.3±3.3 |
| Control group | 37 | 840.5±370.4 | 61.5±4.2 | 515.4±71.2 | 2 | 70.3±16.1 | 8.2±4.5 | 6.4±4.2 |
| T/χ2 | 3.841 | 7.283 | 10.873 | 9.982 | 5.055 | 0.273 | 1.153 | |
| p | 0 | 0 | 0 | 0.001 | 0 | 0.803 | 0.252 |
Table 2: Comparison of Surgical Conditions Between the Two Groups
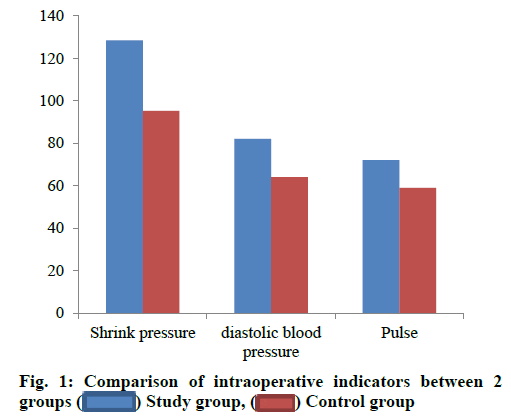
The intraoperative detection results of relevant indexes in the two groups were shown in Table 3 and fig. 1. Compared with the control group, the systolic blood pressure, diastolic blood pressure and pulse level were significantly higher (p<0.05).
| Group | Study group (n=27) | Control group (n=27) | T value | p value |
|---|---|---|---|---|
| Contractile pressure (mmHg) | 128.45±10.26 | 95.26±10.20 | 6.004 | 0.004 |
| Diastolic blood pressure (mmHg) | 82.45±8.26 | 64.23±8.26 | 5.297 | 0.001 |
| Pulse (min) | 72.48±5.29 | 59.48±6.23 | 5.268 | 0.015 |
Table 3: Comparison of Intraoperative Related Indicators Between the Two Groups (χ±s)
The results of adverse reactions in the two groups are shown in Table 4 and fig. 2. Compared with the control group, the incidence of nausea and vomiting, heart rate, blood pressure and chest tightness were significantly lower than those in the control group (p<0.05).
| Group | Study group (n=27) | Control group (n=27) | T value | p value |
|---|---|---|---|---|
| Nausea and vomiting | 1 (3.70) | 2 (7.40) | 6.004 | 0.004 |
| Heart rate increases | 0 (0.00) | 1 (3.70) | 5.297 | 0.001 |
| Blood pressure rises | 1 (3.70) | 2 (7.40) | 5.268 | 0.015 |
| Chest tightness | 0 (0.00) | 1 (3.70) | 5.128 | 0.005 |
| Total occurrence | 2 (7.40) | 6 (22.22) | 5.264 | 0.006 |
Table 4: Comparison of the Incidence of Adverse Reactions Between the Two Groups
The PPP was first proposed by the foreign scholar Chattopadhayay [9]. It refers to those who had a cesarean section last time and this pregnancy was a placenta previa, which is called a pernicious placenta previa (PPP). When the PPP occurs, the placenta is mainly attached to the lower segment of the uterus, causing the lower segment of the uterus to swell and shorten the cervix, making the lower segment of the uterus to be barrel-shaped or gourd-shaped enlargement, and even the ratio of the uterine body to the lower part of the uterus is unbalanced, and the anterior wall muscle layer is thin or even without muscle layer. The placenta is attached to the lower uterine segment, which is often accompanied by penetration of placental implantation, and a large number of angiotensed vessels can be seen in the lower uterine segment during the operation [10].
The lack of smooth muscle in the lower part of the uterus can lead to poor vasoconstriction at the placental attachment site, which in turn causes intraoperative and postoperative bleeding [11]. Placental dissection and extensive bleeding on the wound surface can occur, such as bleeding during uterine placenta dissection or placenta removal, extensive bleeding during abdominal wall scar adhesion to the uterus, bleeding from the posterior wall of the bladder when the adhered bladder is opened, or bleeding from the stump of hysterectomy [12]. Bleeding has the characteristics of extensive small arterial hemorrhage, high vascular pressure, easy re-bleeding of small arteries after folding and suture, difficult to find bleeding sites of leaks and fierce hemorrhage of large arteries. It is also the main cause of postpartum hemorrhage and treatment difficulties [13]. If it is not handled in time, it can cause maternal death. How to reduce intraoperative and postoperative bleeding is an urgent problem to be solved [14]. PPP parturients often bleed a lot in a very short period of time when they terminate pregnancy to remove placenta. In order to avoid uterine hyperinflation and further increase postpartum blood loss, pregnancy can be terminated at 34-36 w of pregnancy. At the same time, multidisciplinary collaboration and individualized treatment should be emphasized [15]. Preoperative ultrasonography, MRI and other examinations should be completed to clarify the involvement of organs near the placenta attachment site and the source of blood supply. A multidisciplinary collaboration team composed of obstetrics, anesthesiology, neonatology, blood transfusion, interventional radiology, urology, intensive care, operating room, etc., shall be established, with doctors who are qualified for perinatal hysterectomy as the surgeons to ensure the smooth operation and reduce surgical complications [16]. In 1997, the British scholar B-Lynch proposed the B-Lynch suture; in 2000, Cho proposed the square suture, in 2005, H Wu et al. proposed the parallel vertical compression suture for the lower segment of the uterus; in 2011, Bao Yirong and Ying Hao proposed the transverse ring compression suture for the lower segment of the uterus, in 2016, Li et al. proposed funnel compression suture, and Yan et al. proposed the annular overlapping suture of the lower uterine segment. In addition, intrauterine balloon placement, iodoform, vaseline gause packing and ligation of internal iliac artery and perioperative pelvic vascular occlusion have also been successively introduced into the treatment of PPP [17,18]. The common features of the above surgical procedures are that suture is performed from serosal membrane to endometrial surface, and uterine compression from the outside to the inside is used to stop bleeding. As suture does not directly involve the bleeding point, incomplete compression and incomplete hemostasis often lead to surgical failure. The hysterectomy rate has been reported as 8 %-11 % [19].
In view of the above-mentioned special anatomical changes, this study proposes the surgical method of multi-directional spiral suture plasty of the lower uterus. The main points of operation are: Start suture from the inside of the uterine cavity. Divide the lower uterine cavity surface into four areas, front, back, left, and right, and perform partial or full lateral narrowing and suture according to the bleeding situation [20,21]. This surgical plan has the following three advantages: The bladder is no longer pushed down, and the operation is simple to avoid extensive bleeding in the uterine bladder adhesion site. Suture the entire lower uterine wound after the placenta has been stripped without affecting the shape of the uterus. The suture will help to restore the normal cervical anatomical shape. All operations are performed on the inside of the uterine cavity, and the bleeding area is directly sutured, without affecting the implementation of supplementary hemostatic programs such as balloon placement and uterine artery ligation [22,23]. The difficulty of this surgical plan is that for parturients with thin anterior wall of the lower uterus or severe adhesion of the uterine bladder, the suture may penetrate the bladder mucosa and cause bladder damage. The operation needs to be cautious [24].
The ergonovine and spiral suture of the lower uterus used in the undergraduate room is based on the unique anatomical changes of the PPP parturients. This surgical program is simple to operate, easy to learn, can quickly and effectively stop bleeding, and help to restore the normal anatomical structure of the lower uterus. At the same time, it does not affect other supplementary hemostatic operations, and provides a good choice for improving the surgical treatment of PPP parturients, which is worthy of clinical promotion [25].
Acknowledgements:
This work was supported by the Affiliated Hospital of Hebei University, Rui Li and Jing Wang contributed equally to this work.
Conflict of Interests:
The authors declared no conflict of interest.
References
- Timor-Tritsch IE, Monteagudo A, Cali G, D’Antonio F, Agten AK. Cesarean scar pregnancy: diagnosis and pathogenesis. Obstet Gynecol Clin North Am 2019;46:797-811.
- Li N, Yang T, Yu W, Liu H, Qiao C, Liu C. The role of Zeb1 in the pathogenesis of morbidly adherent placenta. Mol Med Rep 2019;20:2812-22.
- Cohen B, Wilson M, Cohen A, Yum M. Prenatal diagnosis of a furcate placenta. Obstet Gynecol 2020;135:960-3.
- Cui R, Li M, Lu J, Bai H, Zhang Z. Management strategies for patients with placenta accreta spectrum disorders who underwent pregnancy termination in the second trimester: a retrospective study. BMC Pregnancy Childbirth 2018;18:1-8.
- Isotton AL, Salazar CC, Peralta CF, Abdalla JM, Vettorazzi J. In vitro fertilization and vasa previa: A report of two cases. Rev Bras Ginecol Obstet 2019;41:348-51.
- Papanikolaou IG, Domali E, Daskalakis G, Theodora M, Telaki E, Drakakis P et al. Abnormal placentation: Current evidence and review of the literature. Eur J Obstet Gynecol Reprod Biol 2018;228:98-105.
- Zhang HX, Zhao YY, Wang YQ. Analysis of the characteristics of pregnancy and delivery before and after implementation of the two-child policy. Chin Med J 2018;131:37-42.
- Zhao Q, Zhao N, Luo D, Yue S. Radiologic intervention of internal iliac artery occlusion during cesarean section for dangerous placenta previa. J Med Imaging Health Inform 2020;10:2931-4.
- Velmurugan P, Chattopadhayay AB. Sensitivity analysis of a single phase to ground fault system in connection with high impedance faults: A case study. Cogent Eng 2020;7:1770916.
- Yi XU, Yu W, University XM. Analysis of the effects of lower uterine segment repair in cesarean section of patients dangerous placenta previa. Smart Struct Syst 2019;8:11-20.
- Tian-Jiao Z, Tian-Shi Z, Qing-Yan D. Progress in diagnosis and treatment of different types of dangerous placenta previa. J Drug Target 2019;5(6):120-3.
- Mosconi C, Crocetti L, Bruno A, Candita G, Cappelli A, Perrone O, et al. Scar pregnancy and extrauterine implants. Semin Ultrasound CT MR 2021;42: 46-55.
- Qing-Rong WU, Hao C. Effect of continuous suture of lower uterus on postpartum hemorrhage in cesarean section of scar uterus. Chin J Fam Plann Gynecotokol 2019;27:308-12.
- Savcı G, Ozdemir AZ, Karlı P, Kocak I, Katırcı Y, Onal M. A different method in the treatment of placenta previa: A comparison of lower uterine segment transverse suture technique and Bakri balloon application. Open J Obstet Gynecol 2019;9:334.
- Gan Y, Chen Z, Shi Q. The efficacy between cervical-lifting suture and lower B-Lynch suture in placenta previa: a retrospective cohort-study. Arch Gynecol Obstet 2020;302:365-76.
- Geng-Yan B, Xiao-Min L, Bing LI. Discussion on the value of prenatal ultrasound in diagnosing dangerous placenta previa and placenta accreta. Medicine 2019;12:174-84.
- Tian-Jiao Z, Tian-Shi Z, Qing-Yan D. Progress in diagnosis and treatment of different types of dangerous placenta previa. J Drug Target 2019;8:7-20.
- Ying L, Li-Qiong L, Gui-Li Z. Comparison of clinical characteristics and surgical efficacy between common and dangerous type placenta previa. J Vasc Surg 2019;8:7-20.
- Rong Z, Jin Q I, Ya-Juan Q. Clinical effect of balloon occlusion of abdominal aorta and uterine artery embolization in the treatment of dangerous placenta previa. J Exp Med 2019;16:46-51.
- Brown KG, Di Re A, Fisher D. Suture retraction of the uterus using a percutaneous port closure needle during laparoscopic mesorectal dissection. ANZ J Surg 2020 J;90:1499-500.
- Li XK, Chen J, Wang RC, Li C, Wang M, Liu JH, et al. Early Cretaceous tectonomagmatic evolution and basin development of western Bangong-Nujiang suture: A complete history of soft collision. Lithos 2019;344:360-73.
- Pittman J, Mogensen L, Brannstrom M, Chan W, Morrison N. Uterus transplantation: Perspectives of Australian women with absolute uterine factor infertility regarding desirability and utility. Aust NZJ Obstet Gynaecol 2020;60:264-70.
- Konishi I. Diffuse Leiomyomatosis: complete myomectomy for innumerable small nodules to achieve fertility sparing and childbearing. Surg J 2020;6:S50-7.
- Feng-Liang W, Wei Z. Comparison of different uterine incision suture methods for uterine diverticulum formation during cesarean section. Chin Foreign Med Treat 2019;15:316-20.
- Ping W. Clinical study of carprostol tromethamine combined with mifepristone in the treatment of sinister placenta previa. Contemp Clin Trials 2019;7:20-38.
 Study group,
Study group, Control group
Control group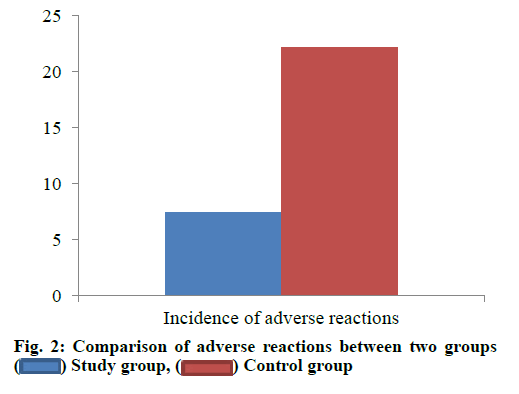
 Study group,
Study group,  Control group
Control group



