- *Corresponding Author:
- Shan Gao
Department of Endocrinology, Affiliated Beijing Chaoyang Hospital of Capital Medical University, Beijing 100043, China
E-mail: zbb7546846@163.com
| This article was originally published in a special issue, “Clinical Research in Pharmaceutical and Biomedical Sciences” |
| Indian J Pharm Sci 2021:83(1)spl issue “181-187” |
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms
Abstract
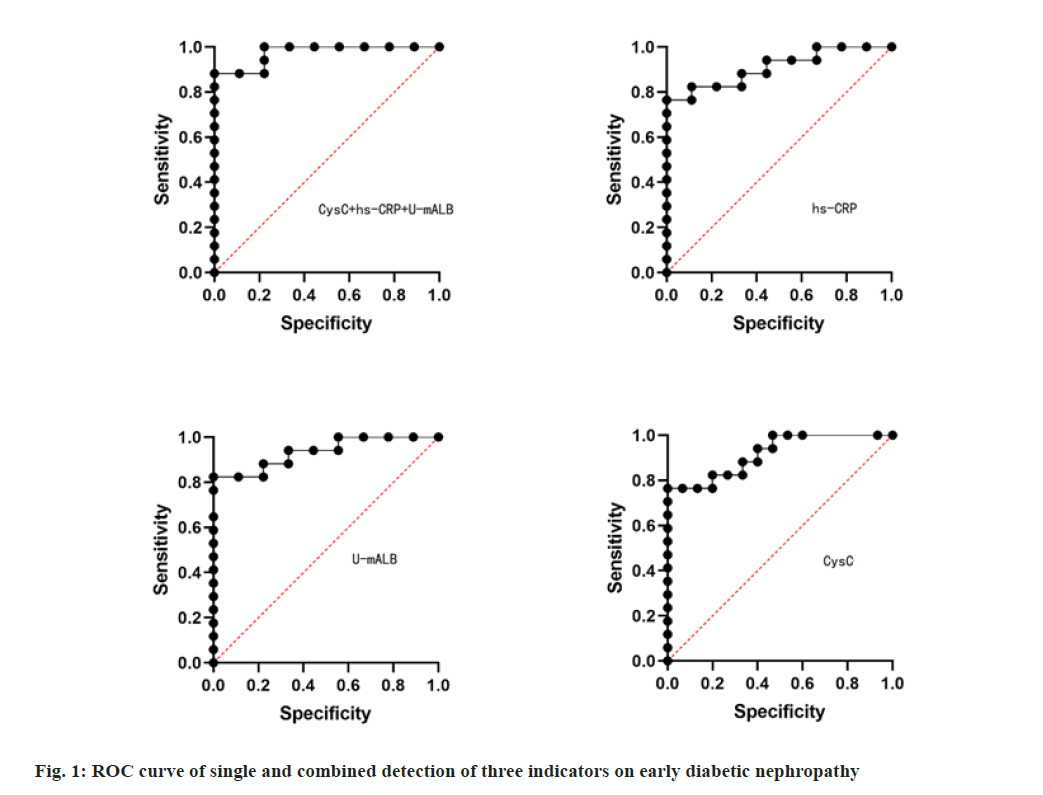
To explore the value of combined detection of cystatin C, high sensitivity C-reactive protein and microalbuminuria in the diagnosis of early diabetic renal damage. From September 2016 to May 2018, 96 patients with type 2 diabetes were selected and divided into three groups according to the staging criteria of renal damage caused by diabetes: simple diabetes group (32 cases), early diabetic nephropathy group (32 cases) and clinical diabetic nephropathy group (32 cases). Another 32 healthy people in the same period were selected as the control group. Fasting venous blood and urine were collected to detect microalbuminuria, urine microalbuminuria, serum cystatin C and hypersensitive C-reactive protein. The sensitivity and specificity of three detection indexes were analyzed by receiver operating characteristic curve. Compared with the control group, the levels of cystatin C, high sensitivity C-reactive protein and microalbuminuria in the simple diabetic group, the early diabetic nephropathy group and the clinical diabetic nephropathy group were significantly increased (p<0.05); the levels of cystatin C, high sensitivity C-reactive protein and microalbuminuria in the early diabetic nephropathy group and the clinical diabetic nephropathy group were significantly higher than those in the simple diabetic group (p<0.05).In the early diabetes group, the positive rates of cystatin C, high sensitivity C-reactive protein and microalbuminuria were lower than those of combined detection, and the difference was statistically significant (p<0.05). Receiver operating characteristic curve analysis showed that the Area under the curve of microalbuminuria, whole blood high sensitivity C-reactive protein, serum cystatin C and diagnosis of early diabetic nephropathy were 0.960, 0.934 and 0.929 respectively, with high accuracy. The AUC of combined detection of the three indicators was 0.994, with sensitivity and specificity of 100.00 % and 99.70 %. The combined detection of high sensitivity C-reactive protein, microalbuminuria and serum cystatin C can improve the sensitivity and specificity of diagnosis of early diabetic nephropathy, which is of great significance for clinical prevention and treatment of early diabetic nephropathy and progression to end-stage renal disease.
Keywords
Diabetes mellitus, early renal injury, high sensitivity C-reactive protein, microalbuminuria, cystatin C
Diabetes is one of the main diseases that seriously threaten human health. With the continuous improvement of living standards, the aging of the population and the change of lifestyles, the incidence of diabetes is increasing year by year. According to the World Health Organization report, the number of diabetic patients worldwide till 2030 will reach 3.66 billion and the number of Chinese patients will reach 420 million[1]. Diabetic nephropathy (DN) is one of the common and serious microvascular complications of diabetes and one of the main life-threatening causes. Due to the insidious onset of the disease, when the clinical manifestations are obvious proteinuria, edema, diabetes and renal insufficiency, the disease has become serious and preventive treatment is no longer possible. However, DN can be reversed after early clinical intervention[2]. Therefore, it is of great significance to determine the early renal damage of diabetes. In recent years, some studies have shown that serum cystatin C (Cys-C) is a good serum marker that reflects impaired glomerular filtration function[3]; hypersensitive C-reactive protein (hs-CRP) is also a sensitive marker of early renal damage[4,5]; urine microalbuminuria(U-mAlb) is the first clinical signal of diabetes, and its value in monitoring early renal damage of diabetes has been recognized. At present, there are few studies on the combined detection of the above three indicators for early diabetic renal damage diagnosis. Based on this, this study investigated the expression levels of U-mAlb, serum Cys-C, whole blood hs-CRP and in early diabetic renal damage, and analyzed the diagnostic value of the combined detection of the three indexes in early diabetic renal damage, to provide reference for clinical disease prevention and treatment. A total of 96 patients with type 2 diabetes admitted to our hospital from September 2016 to May 2018 were selected, including 48 male patients and 38 female patients, aged 42-78 y, with an average age of (51.20±4.30) y. According to the classification criteria of diabetes renal damage, the patients were divided into three groups: simple diabetic group (32 cases), early diabetic nephropathy group (32 cases), and clinical diabetic nephropathy group (32 cases). In addition, 32 healthy subjects in the same period were selected as the control group, including 19 male patients and 13 female patients, aged 45-72 y, with an average age of (50.85±5.11) y. There was no statistically significant difference in baseline data such as gender and age among the three groups (p>0.05). Inclusion criteria for this study: Patients of early diabetic nephropathy group were clinically diagnosed with early diabetic renal damage, patients in the simple diabetic group and clinical diabetic nephropathy met the diagnostic criteria for diabetes, and the case data of all patients were complete; Patients were willing to bear relevant risks of the study, signed informed consent and are initiative to accept relevant examinations of the research; Exclusion criteria: Patients with other systemic immune diseases, such as systemic lupus erythematosus, systemic purpura, acquired immunodeficiency syndrome, etc.; Patients with other tumor related diseases, such as liver cancer, gastrointestinal mass, lung cancer, brain tumor, etc.; Patients with severe mental disorders such as schizophrenia, severe depression, or severe mania which make them difficult to cooperate with inspection workers; Patients with severe diabetes or coronary heart disease. Fasting venous blood 6 ml in the morning was collected from the subjects, of which 4 ml was placed in the separator gel/coagulant tube for centrifugation at 3000 r/min for 10 min. The serum was separated and frozen at -20° for examination. The other 2 ml was placed in the routine blood tube and the test was completed within 2 h. At the same time, 10 ml of morning urine was taken from the subjects and placed in the urinary catheter for immediate examination. The test was completed within 2 h after centrifugation at 3000 r/min for 5 min. The whole blood hs-CRP (emulsion immunoturbidimetric method) was determined by the Minray BC-53930 CRP automatic blood cell analyzer, and the U-mAlb (immunoturbidimetric method) and serum Cysc (particle enhanced immunotransmission turbidimetric method) were determined by the Beckmann Coulter AU5800 automatic biochemical analyzer. The reagents were purchased from Jinhua Qiangsheng Biotechnology Co., Ltd. The above operations are strictly carried out in accordance with the reagent instructions. U-mAlb standard value≤25 mg/l, whole blood hs-CRP standard value≤25 mg/l, serum Cysc standard value ≤1.4 mg/l. If the result is higher than the standard value, it is positive. If the result of any one item is higher than the standard value in the combine detection, it is positive. SPSS19.0 software was used for statistical analysis. Measurement data were expressed as x±s. Two-sample t test was used for comparison between groups. Enumeration data were compared by χ2 test. Pearson correlation was used for correlation analysis. p<0.05 was considered statistically significant. Compared with the control group, Cysc, hs-CRP and U-mAlb were significantly increased in the simple diabetic group, early diabetic nephropathy group and clinical diabetic nephropathy group, with statistical significance (p<0.05). Serum Cys-C, hs-CRP and U-mAlb in early diabetic nephropathy group and clinical diabetic nephropathy group were significantly higher than those in simple diabetic nephropathy group, and the difference was statistically significant (p<0.05). See Table 1 for specific data.
| Group | Cases | CysC (mg/L) | Hs-CRP(mg/L) | U-mAlb (mg/L) |
|---|---|---|---|---|
| Control | 32 | 0.76±0.21 | 0.72±0.16 | 12.08±3.02 |
| Simple diabetic | 32 | 1.65±0.54* | 1.12±0.35* | 17.53±4.84* |
| Early diabetic nephropathy | 32 | 2.47±0.69*# | 2.74±0.72*# | 26.36±3.88*# |
| Clinical diabetic nephropathy | 32 | 3.52±0.61*# | 4.68±1.58*# | 42.37±14.16*# |
Note: Compared with the control group, *p<0.05; Compared with the single diabetic group, #p<0.05.
Table 1: Comparison of Test Results in Each Group
The positive rates of CYSC, hs-CRP and U-mAlb by single test were lower than those by combined test, and the difference was statistically significant (p<0.05). Table 2 was provided with specific data. receiver operating characteristic curve (ROC curve) analysis showed that AUC of U-mAlb, hs-CRP, the whole blood serum CysC in diagnosis of early diabetic nephropathy were 0.935, 0.918, 0.909, and the accuracy is high, The above three indicators were included in the Logistic regression model, and the data of the combined detection of the three indicators were obtained through the regression coefficient. Further ROC curve analysis showed that the AUC of the combined detection of the three indicators was 0.974, and the sensitivity and specificity were 100.00 % and 97.40 %, both of which were higher than that of any single detection of the three indicators, indicating the high value of the combined detection. See fig. 1 and Table 3. With the improvement of people’s living standards, the incidence of diabetes is also increasing. Diabetic nephropathy has now become the first primary disease of chronic renal failure in developed countries, and the incidence rate in China is also rising rapidly[6]. Diabetic nephropathy is a chronic process, and its early clinical manifestations are not obvious. The routine urine protein examination is mostly negative, and once it develops to end-stage renal disease, the treatment is often more difficult than other renal diseases[7]. Therefore, early diagnosis and timely prevention are of great significance for delaying diabetic nephropathy.
| Group | Cases | Positive freuency | Positive rates |
|---|---|---|---|
| CysC | 32 | 15 | 46.88 |
| Hs-CRP | 32 | 14 | 43.75 |
| U- mAlb | 32 | 16 | 50.00 |
| Combined test | 32 | 26 | 81.25* |
Note: compared with other single tests, *p<0.05
Table 2: Single and Combined Positive Detection Rates of Cys C, Hs-Crp and U-Malb in Early Diabetic Nephropathy Group
| Sensitivity (%) | Specificity | |
|---|---|---|
| U-mALB | 88.5 | 0.935 |
| hs-CRP | 90.6 | 0.918 |
| CysC | 85.5 | 0.909 |
| Combined detection | 100 | 0.974 |
Table 3: Diagnostic Sensitivity and Specificity of Single and Combined Detection of Three Indicators for Early Diabetic Nephropathy
Cystatin C is widely present in body fluids and cells of various tissues throughout the body. The serum concentration of Cystatin C is relatively stable and is not easily affected by drugs, inflammation, diet, muscle mass, etc., and is mainly excreted through the kidneys, which is a good indicator of glomerular filtration rate. At present, Cystatin C has been used in the evaluation of renal function after kidney transplantation[8], diabetic nephropathy[9] and the early damage of acute kidney injury[10]. These studies believe that the detection of renal function by serum cystatin C reflects the decrease in glomerular filtration rate earlier than serum creatinine or urea nitrogen, and has better specificity and sensitivity, and can replace serum creatinine or urea nitrogen as new indicators for kidney function testing. However, related literature reports indicate that the content of cystatin C in the serum of patients with coronary heart disease is significantly increased[11], so the interference caused by coronary heart disease should be excluded during testing. The content of hs-CRP in the normal body is few, it is synthesized by the liver, and has a short half-life. When patients have inflammatory infection, hs-CRP will increase, and early renal injury in diabetes can lead to the increase of inflammatory factors[12]. Under normal conditions, the level of U- mAlb in urine is low, but when the glomerulus is damaged, its volume barrier and charge barrier are destroyed, which can lead to abnormal increase of U-mAlb excretion, which can be used as a sensitive indicator for the diagnosis of early renal injury[13-15]. The results of this study showed that the concentrations of Cysc, hs-CRP and U-mAlb in diabetic nephropathy patients were significantly higher than those in normal healthy population. In addition, this study also found that the concentrations of Cys-C, hs-CRP and U- mAlb increased with the increase of renal function impairment in diabetic nephropathy, which indicated that Cysc, hs-CRP and U-mAlb had a high specificity for renal function impairment in diabetic nephropathy patients and could reflect the degree of renal function impairment in the body. The results of this study showed that the positive rate of the combined detection of three indicators in the early diabetic group was significantly higher than that of the single detection of U- mAlb, whole blood hs-CRP and serum Cysc, indicating that the combined detection of three indicators had better diagnostic value for diabetic nephropathy. Further analysis of ROC curve showed that in the diagnosis of diabetic nephropathy, the AUC of U-mAlb was 0.935 and its sensitivity was 88.5%; the AUC of whole blood hs-CRP was 0.918, and its sensitivity was 90.6 %; serum CysC diagnosis of diabetic nephropathy AUC is 0.909, its sensitivity was 85.5 %, suggesting that the accuracy of the single detection of three indicators are both high, the diagnostic sensitivity: whole blood hs-CRP>U- mAlb>serum CysC. The results of domestic studies also pointed out that the diagnostic sensitivity of U-mAlb>CysC. This suggests that regular U- mAlb testing can help find kidney damage in time[12]. However, studies have pointed out that U-mAlb test results can be affected by factors such as exercise. CysC can only be metabolized by the kidneys. When the body has minor glomerular damage, the level of CysC rises, and the sensitivity of the diagnosis of kidney injury is high. It can make up for missed diagnosis caused by U-mAlb[15]. The results of this study show that the combined detection of hs- CRP, U-mAlb, and serum CysC in whole blood has an AUC value of 0.994, which has high accuracy for the detection of early diabetic nephropathy, and can improve the sensitivity and specificity of diagnosis It was of great significance to prevent happening of early renal injury and even progression to end-stage renal disease in diabetic patients.
Therefore, it is found that the chondrorepair activity of progenitor cells can be stimulated by the modification of various genes in stem cells by the independent gene transduction of slow virus vector, which provides the basis for controlling the cartilage repair process after hADSCs are implanted into cartilage defects.
The benefit of co-transduction of therapeutic lentiviral vector gene repairer hADSCs provides evidence that enhancing the expression of Sox9 and knockdown β-catenin can significantly improve its cartilage repair activity in vitro.
Acknowledgments:
This work was supported by the Affiliated Beijing Chaoyang Hospital of Capital Medical University.
Conflict of Interests:
The authors report no conflicts of interest.
References
- Jin H. Increased levels of glycosylated hemoglobin, microalbuminuria and serum cystatin C predict adverse outcomes in high-risk pregnancies with gestational diabetes mellitus. Exp Ther Med 2020;19(2):1281-7.
- Kim HJ, Byun DW, Suh K, Yoo MH, Park HK. Association between serum cystatin c and vascular complications in type 2 diabetes mellitus without nephropathy. Diabetes Metab J 2018;42(6):513.
- Kobayashi T, Yokokawa H, Fujibayashi K, Haniu T, Hisaoka T, Fukuda H, et al. Association between high cystatin C levels and carotid atherosclerosis. World J Cardiol 2017;9(2):174.
- Li H, Gao F, Xue Y, Qian Y. Value of plasma growth differentiation factor-15 in diagnosis and evaluation of type 2 diabetic nephropathy. J South Med University 2014;34(3):387-90.
- Lu YA, Li W. Relationship between Serum Cystatin C and Vascular Complications in Type 2 Diabetes Mellitus Patients with Normal Renal Function. Acta Academy Med Sci 2020;42(6):795-800.
- Lum G. How effective are screening tests for microalbuminuria in random urine specimens?. Annal Clin Lab Sci 2000;30(4):406-11.
- Rashad NM, El-Shabrawy RM, Sabry HM, Fathy HA, Said D, Yousef MS. Interleukin-6 and hs-CRP as Early Diagnostic Biomarkers for Obesity-Related Peripheral Polyneuropathy in Non-Diabetic Patients. Egyptian J Immunol 2018;25(2):153-65.
- Wang L, Wu J, Cheng JF, Liu XY, Ma F, Guo LH, et al. Diagnostic value of quantitative contrast-enhanced ultrasound (CEUS) for early detection of renal hyperperfusion in diabetic kidney disease. J Nephrol 2015;28(6):669-78.
- Xu LL, Gao W, Chen ZM, Shao KK, Wang YG, CUI L, et al. Relationships between diabetic nephropathy and insulin resistance, inflammation, Trx, Txnip, CysC and serum complement levels. Eur Rev Med Pharm Sci 2020;24(22):11700-6.
- Yang H, Xu W, Zhou Z, Liu J, Li X, Chen L, et al. Curcumin attenuates urinary excretion of albumin in type II diabetic patients with enhancing nuclear factor erythroid-derived 2-like 2 (Nrf2) system and repressing inflammatory signaling efficacies. Exp Clin Endocrinol Diabetes 2015;123(6):360-7.
- Yang X, Lin Q, Li X, Wu L, Xu W, Zhu Y, et al. Cystatin C Is an Important Biomarker for Cardiovascular Autonomic Dysfunction in Chinese Type 2 Diabetic Patients. J Diabetes Res 2019;2019.
- Zakariah NA, Bajuri MY, Hassan R, Ismail Z, Mansor MM, Othman H, et al. Is Procalcitonin more superior to hs-CRP in the diagnosis of infection in diabetic foot ulcer? Malaysian J Pathol 2020;42(1):77-84.
- Zhao W, Pan J, Li H, Huang Y, Liu F, Tao M, et al. Relationship between high serum cystatin C levels and the risk of gestational diabetes mellitus. PloS one 2016;11(2):e0147277.
- Zhao Y, Liu J, Ten S, Zhang J, Yuan Y, Yu J, et al. Plasma heparanase is associated with blood glucose levels but not urinary microalbumin excretion in type 2 diabetic nephropathy at the early stage. Renal Failure 2017;39(1):698-701.
- Zhu M, Lin J, Wang C, Yang M, Lv H, Yang M, et al. The relationship among angiotensinogen genes polymorphisms and hs-CRP and coronary artery disease. J Clin Lab Anal 2019;p33(5):e22881